This story contains descriptions of stillbirths.
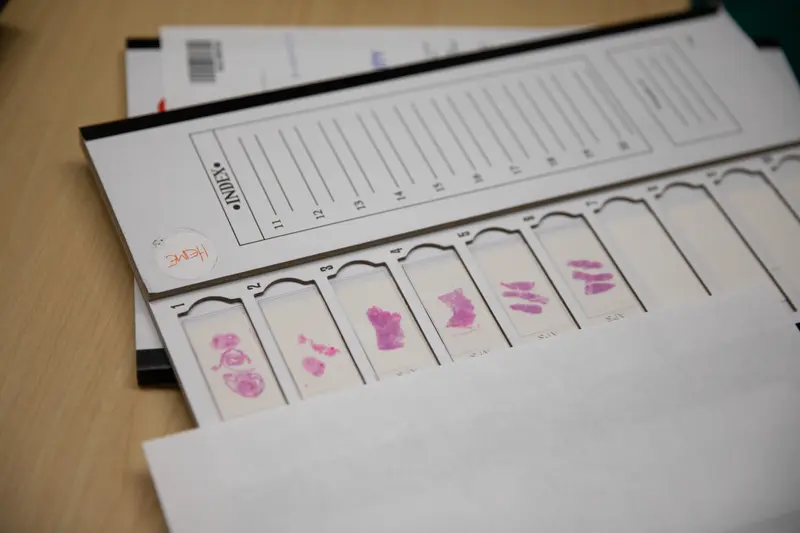
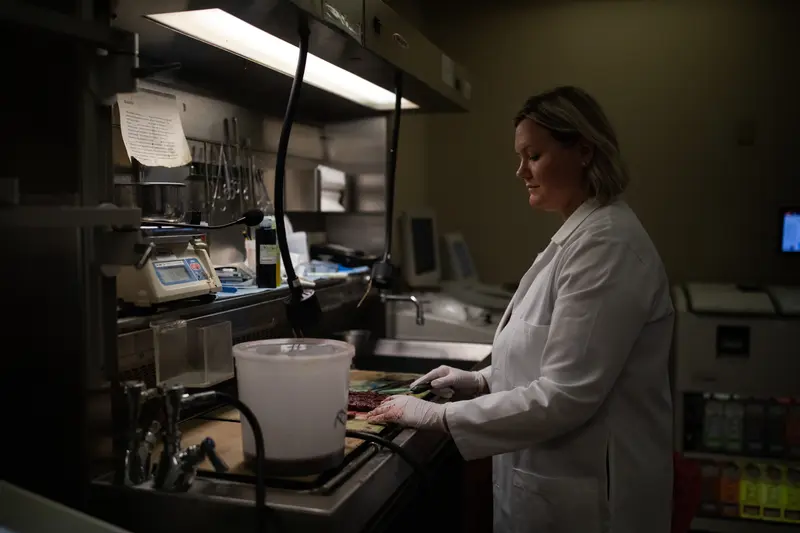
Late one afternoon last October, Dr. Shelley Odronic sat in her office and, just as she had thousands of times before, slid a rectangular glass slide onto her microscope.
A pathologist who works in rural Ohio, Odronic leaned forward to examine tissue from the placenta of a woman who had recently given birth. She increased the magnification on the microscope. Never had she seen so many tiny, congealed reservoirs of blood or such severe inflammation of the tissue, a sign the placenta had been fighting an infection.
“Right away, I knew it wasn’t compatible with life,” Odronic said.
She asked her secretary to print out the patient’s chart. In dark letters were the words “fetal demise.” A stillbirth, the death of a fetus at 20 weeks or more of pregnancy. But that didn’t solve the mystery. Odronic had examined many placentas from pregnancies that ended in stillbirth. None looked like this — withered and scarred.

Odronic kept reading. No chronic medical conditions. Good prenatal care. Then, buried in the middle of the report, she spotted something. Seven days before the stillbirth, the mother had tested positive for COVID-19. Odronic wondered if the virus could explain the damage to the placenta. In the world of placenta pathology, a new affliction is unusual, especially one so dramatic in presentation and so devastating in effect.
Her mind traveled to Dr. Amy Heerema-McKenney, a pathologist at Cleveland Clinic and an expert on the placenta, who had trained Odronic during residency. Odronic went to sleep that night with a pit in her stomach and a plan to call her former teacher in the morning.
Heerema-McKenney was in her office when the phone rang. As she listened, she knew that what Odronic was describing was what she and her colleagues had observed repeatedly over the past several months: a patient positive for the coronavirus, a placenta destroyed by COVID-19, a baby stillborn.
Their next discovery was equally stunning. None of the stillbirths they studied involved a pregnant person who had been fully vaccinated. The doctors checked with colleagues across the country and around the world. The fatal pattern held.

Unvaccinated women who contracted COVID-19 during pregnancy were at a higher risk of stillbirths. They also were more likely to be admitted to the intensive care unit, give birth prematurely or die. Yet their greatest protection — the COVID-19 vaccine — sat largely untouched, buried under doubt, polluted by disinformation.
Pharmaceutical companies and government officials failed to ensure that pregnant people were included in the early development of the COVID-19 vaccine, a calamitous decision made amid the urgency of a rapidly spreading pandemic. That decision left pregnant people with little research to rely on when making a critical decision on how best to keep the babies growing inside of them safe.
At the same time that research was excluding pregnant people from vaccine trials, a full-scale assault on vaccination was unfolding online. Taking advantage of the lack of data, conspiracy theorists, anti-vaxxers and even some medical professionals spread false claims about the vaccine’s safety in pregnancy, leading many pregnant people to delay or refuse the vaccine. Even now, with numerous studies unequivocally announcing the safety of the vaccine for pregnant people, some doctors have failed to communicate the dangers of COVID-19 to pregnant people or the vaccine’s role in mitigating it.
The Centers for Disease Control and Prevention contributed to the confusion with vague early messaging about whether pregnant people should get vaccinated. While Americans lined up at pharmacies and stalked vaccine websites in hopes of securing a shot last year, pregnant people had some of the lowest vaccination rates among adults, with only 35% fully vaccinated by last November. Meanwhile, many Americans were already moving on to their boosters after federal officials that month expanded eligibility for the additional shots to anyone 18 or older. And much of the country was beginning to return to pre-pandemic life. The Sunday after Thanksgiving, for instance, set the record for the busiest day of air travel since March 2020.
November also marked a key moment in the understanding of COVID-19’s impact on stillbirths. A CDC study looking at 1.2 million births in the first 18 months of the pandemic found that more than 8,000 pregnancies ended in stillbirths, including more than 270 of them in patients with a documented COVID-19 diagnosis at the time of delivery.
Although stillbirths were rare overall, babies were dying. The risk of a stillbirth nearly doubled for those who had COVID-19 during pregnancy compared with those who didn’t. And during the spread of the delta variant, that risk was four times higher.

Indeed, doctors discovered that some stillbirths resulted from COVID-19 directly infiltrating the placenta, a condition they named SARS-CoV-2 placentitis. Cases were found even in people whose COVID-19 symptoms were mild or nonexistent. In some cases, however, placentas were discarded with medical waste without being tested for COVID-19, and parents never learned what led to their baby’s stillbirth.
COVID-19 also led to stillbirths among pregnant people who became exceedingly ill after contracting the virus. It damaged their lungs and clotted their blood, putting their babies in such severe distress that they were born before they could take their first breath.
“These are pregnancies that should not have ended,” Heerema-McKenney said.
She and others had tried to alert the CDC as well as maternal and state health organizations to their findings, but she said they either didn’t get a response or were told they needed to collect more data and publish studies. Pathologists are experts in disease diagnosis, dealing with death and illness from the safe distance of their labs. Convincing obstetricians who met with patients daily or doctors who were making policy recommendations was a challenge.
“I tried to sound the alarm. We tried so hard to get people to listen,” Heerema-McKenney said. “It was a really frustrating place to be as pathologists doing these autopsies, looking at these placentas and saying, ‘God, no, not another case.’”
Around the same time Heerema-McKenney was examining the damaged placentas, Ginger Munro was on life support in a hospital 250 miles away in another part of Ohio.
She and her husband, Kendal, had been trying to have a child for five years. They hadn’t expected that she’d get pregnant in the middle of a pandemic. But when her pregnancy test came back positive in the spring of 2021, she rushed to post a picture of it in an online pregnancy group. “Is it just me or can you see the 2 lines??” she asked.
The pandemic had already brought much change to their lives. Ginger, who lives in the small town of Washington Court House in southwest Ohio, quit her job as assistant nutrition director with the county’s Commission on Aging. She stationed hand sanitizer throughout her house and in her car, and she only went grocery shopping early in the morning. If she noticed someone in an aisle, she skipped it.
“I knew the virus was real,” she said, “but I was terrified to take the vaccine.”

Ginger worried that the vaccine’s development had been rushed, and she hadn’t seen any data showing it was safe for pregnant people. At this point, the CDC had not explicitly recommended the vaccine during pregnancy. Ginger already worried she was tempting fate by getting pregnant at 40; she said she didn’t want to risk endangering her baby by taking the vaccine.
Besides, if it was really important, her doctor would have mentioned it, and, she said, she would have followed his advice. But, she said, he never did. Her family hadn’t gotten vaccinated either. In a mostly rural county where less than half of the residents were vaccinated, they were hardly alone.
Her doctor declined to comment through a spokesperson at the hospital system where he works; the spokesperson said the hospital couldn’t disseminate information about the vaccine to pregnant patients before it was recommended.
Ginger’s pregnancy progressed without complications. She and Kendal shared the news of a new baby with Ginger’s two daughters from a previous marriage. At their kitchen table, near a sign that read “eat cake for breakfast,” Sophia, then 14, covered her mouth with both hands while Hailee, then 18, simply beamed.
At a backyard gender reveal three months later, Ginger’s growing belly resembled a basketball against her tiny frame. She leaned in to kiss her husband, her long, dark hair falling onto her shoulders. Red confetti rained down on the deck.
Kendal, an aircraft maintenance and avionics manager at an airport two counties away, worked through the pandemic. In the summer, when they realized his cough was actually COVID-19, it was too late. Ginger was sick.
Having trouble reaching her doctor, she went to two different emergency rooms. One, she said, declined to treat her with monoclonal antibodies, which research had shown can be an effective treatment for pregnant people with COVID-19. The other, which described her in medical records as “an exceedingly pleasant individual admitted with symptomatic COVID-19 pneumonia,” transferred her about an hour away to the University of Cincinnati Medical Center. There, records show, she was admitted with acute respiratory distress syndrome due to COVID-19.
The University of Cincinnati doctor asked Ginger and Kendal — who was on FaceTime because of the hospital’s COVID-19 protocols — about “fetal priority.” Ginger made her wishes clear: Save the baby, their baby, the baby they had tried so hard to have. Kendal, who was worried about both his wife and their unborn child, said he went along with Ginger in that moment.
“You were so scared,” Kendal wrote in a notebook that night. “We told each other over and over how much we loved each other.”
They hung up so the doctors could insert a breathing tube. Before they could begin, Kendal called back three more times just to hear her voice.
Doctors put Ginger on ECMO, a form of life support reserved for the sickest patients. Kendal, Hailee, Sophia and Ginger’s mother and sister were later allowed in the hospital two at a time, and they prayed at her bedside nearly every night. Ginger was sedated, her face swollen and obscured by tubing, her cheeks flattened by the crush of the ventilator straps, her wrists tied down so she wouldn’t accidentally pull out her breathing tube.
Her family took solace in knowing the baby’s heartbeat was steady and her ultrasounds were normal. The doctors gave Ginger medication to help the baby’s lungs mature in case she was born early. After more than 30 days on ECMO, doctors took Ginger off the machine only to put her back on the next morning. She was the first patient in the hospital’s history to be placed on ECMO twice.
The plan, records show, was to deliver at 28 weeks. But the day after Ginger was put back on life support, Kendal got the call telling him the baby was on her way. As doctors prepared for the delivery in Ginger’s intensive care room, the family camped out in the waiting room, jittery from excitement and vending machine snacks. They talked about baby names and future family outings. They pulled the waiting room chairs together to form makeshift beds and covered themselves with blankets they brought from home.
They don’t know if they actually fell asleep before a nurse burst through the doors screaming at them to follow. “She’s coming! She’s coming!” They didn’t make it far before they were blocked by doctors and nurses, some huddled over an incubator in the middle of the hall and the rest crowded around Ginger.
Hailee tried to peer over the sea of blue scrubs to catch the first glimpse of her little sister. She smiled beneath her black mask. She’ll be OK, she said to herself.
But after a few minutes of trying to revive the baby, a doctor told Kendal it was time. Kendal nodded, asked for a chair and collapsed as he tried to process his daughter’s death.
Then another wave of grief washed over him. Someone would have to tell Ginger.
Content Warning
Warning: The following image shows a stillborn baby. The Munro family had photos taken of their daughter to preserve their memory of her.

Ginger’s medical records describe a baby born at 27 weeks “without signs of life” after an “uncomplicated delivery.” Her placenta had separated from the wall of the uterus, the risk of which studies have shown increases with COVID-19.
When Ginger woke up, she looked down at her sunken belly and realized she had given birth. She assumed her daughter was in the newborn intensive care unit. Ginger was barely able to speak around the tube in her trachea, but after a few days in which no one brought the baby to her, she couldn’t wait any longer. Ginger turned to her mother and sister and mouthed the words, “Where’s the baby?”
The room fell silent. They called Kendal, who rushed to the hospital. He told her what had happened. He described their daughter’s dark hair and her long fingers and toes, just like her mother’s.
Ginger, who had always loved the sweet smell of a newborn’s breath, whispered to her husband.
“Did you smell her breath?”
“She wasn’t breathing,” he said.

In the hurried quest for a safe and effective COVID-19 vaccine, pharmaceutical companies and government officials did not include pregnant people in their initial plans. It’s a failure that continues to reverberate.
“They absolutely should have been included in COVID vaccine trials from the beginning,” said Kathryn Schubert, president and CEO of the Society for Women’s Health Research, a Washington, D.C.-based nonprofit that advocates for the inclusion of women in research and clinical trials.
Researchers and advocates have spent more than four decades trying to dismantle the belief that it’s unsafe or unethical for pregnant women to participate in clinical trials. A couple years ago, it seemed like they had finally prevailed.
Shortly before leaving office, President Barack Obama signed into law the 21st Century Cures Act, which established the Task Force on Research Specific to Pregnant Women and Lactating Women. The group found longstanding obstacles, including liability concerns, to including pregnant and lactating people in clinical research. It concluded that recommending halting medication or forgoing treatment while pregnant may actually endanger the health of the mother and her fetus more than the treatment itself.
The need for everything from asthma to depression medication doesn’t stop when a person gets pregnant, and when a catastrophic event such as a pandemic hits, experts said, pregnancy should not preclude someone from receiving life-saving treatment.
Around the same time, researchers discovered that the Zika virus, which was mainly transmitted through mosquitoes, could pass from a pregnant person to their fetus and cause severe birth deformities. A second group of experts joined together to develop separate guidance on including pregnant people in the research, development and deployment of pandemic vaccines.
Both groups pushed to remove pregnant women from a list of vulnerable populations that required additional review before being allowed to participate in research. Instead of proving that pregnant women should be included, manufacturers would need to provide compelling evidence for why they shouldn’t.
In 2018, the federal task force issued recommendations calling for including pregnant and breastfeeding people in biomedical research, and the Department of Health and Human Services adopted some of the guidance. But a gap remained between what the task force and others insisted was needed and what was actually happening.
“We were frustrated because COVID-19 provided an opportunity to implement the recommendations of the task force,” said Dr. Diana Bianchi, the director of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the chair of the task force.
In February 2021, Bianchi and her colleagues published an article lamenting the exclusion of those who were pregnant or breastfeeding from the initial COVID-19 vaccine clinical trials. “Pregnant and lactating persons should not be protected from participating in research, but rather should be protected through research,” they wrote.
Ruth Faden, the founder of the Johns Hopkins Berman Institute of Bioethics, helped lead the group that issued the guidance after Zika. She and others urged manufacturers to include pregnant people in the development of the COVID-19 vaccine as part of Operation Warp Speed, the federal program that provided billions of taxpayer dollars to pharmaceutical companies to speed up vaccine production.
“There is a playbook in place so that when the U.S. launches Operation Warp Speed, it should be pretty obvious what should be done,” she said. “It’s not like no one knows how to do this, either ethically or technically.
“Nevertheless, it doesn’t happen,” Faden added. “Once again, pregnant people are left behind.”
A spokesperson for Pfizer said the company followed guidance from the Food and Drug Administration. Although pregnant people were not included in the initial vaccine clinical trials, Pfizer tested its vaccine on pregnant rats and did not identify any safety concerns. The company subsequently launched a clinical trial with pregnant women but halted it because at that point the vaccine had already been recommended for pregnant people.
Similarly, Moderna also studied its vaccine on pregnant animals, but the company said it made the decision “to prioritize the study of the safety and efficacy” of the vaccine in adults who weren’t pregnant. It called that approach “consistent with the precedent to study new vaccines in pregnant women only after demonstration of favorable benefit and risk in healthy adults.”
In response to questions from ProPublica, Johnson & Johnson referred a reporter to its website, which didn’t address the relevant issues.
Some government officials, including several from the Food and Drug Administration, said they support having pregnant women take part in clinical studies of vaccines for emerging infectious disease, including COVID-19. A spokesperson for the National Institute of Allergy and Infectious Diseases, which is part of the National Institutes of Health, said the agency did not “dictate the protocol development” for the trials and said that responsibility lies with the companies.
The failure to include pregnant people early on in COVID-19 vaccine trials was, at least in part, a casualty of the tremendous urgency to respond to an intense public threat and develop the vaccine as quickly as possible, Faden said. But multiple groups had published road maps on how to ethically include pregnant people without slowing down that process.
“I can’t tell you how many pregnant people might not have died or how many stillbirths might not have occurred if the playbook had been followed,” she said, “but I’m willing to bet it was a significant chunk that would have been prevented if there had been a full-throated, evidence-based recommendation for COVID-19 vaccines in pregnancy almost simultaneous to when it was available for the rest of the adult population.”
By the time the CDC specifically recommended the vaccine for pregnant people, in August 2021, the damage had been done.
A dizzying and vague series of advisories led to confusion and delayed vaccinations. When the COVID-19 vaccines were first made available in December 2020, the CDC said health care workers and residents of long-term care facilities should be prioritized, but the shots were not explicitly recommended for pregnant people. Instead, the agency said on its webpage for vaccines and pregnancy that pregnant health care workers “may choose to be vaccinated.” In explaining that decision, the CDC said that experts had considered how mRNA vaccines, which do not contain the live virus, work. They concluded that the vaccines “are unlikely to pose a risk for people who are pregnant.”
“However,” the CDC added, “the potential risks of mRNA vaccines to the pregnant person and her fetus are unknown because these vaccines have not been studied in pregnant women.”
In January, the World Health Organization recommended against pregnant people getting the vaccine unless they faced increased risk, such as complicating comorbidities or exposure to the virus due to a job in health care, but the agency later reversed course.
A few months later, in March 2021, the CDC continued its lukewarm messaging that pregnant people “may choose” to be vaccinated. The agency listed some points for pregnant people to consider discussing with their health care providers, starting with how likely they are to be exposed to COVID-19.
After a promising study showed that the vaccine was safe for pregnant people, CDC Director Dr. Rochelle Walensky said at a White House briefing in late April that the CDC was recommending the vaccine for them. But the CDC did not update its website to reflect her comments and said the agency’s guidance had not changed: Pregnant people “may choose to be vaccinated.”
Once again, pregnant people were put in the precarious position of receiving ambiguous and inconsistent recommendations. In May 2021, the CDC reiterated that pregnant people faced an increased risk of getting severely ill from COVID-19, but the language surrounding the vaccine — “If you are pregnant, you can receive a COVID-19 vaccine” — was noncommittal.
A CDC spokesperson, responding to questions from ProPublica, said in an email that pregnant people were part of the first recommendations in December 2020 that encouraged people 16 and older to get vaccinated. At that time, data about the safety and efficacy of the vaccine during pregnancy was limited “because pregnant people had been excluded from pre-authorization clinical trials,” so the CDC included additional supporting language for pregnant people, saying they were eligible and could choose to receive the vaccine. The agency said its recommendations were based on available evidence and evolved throughout the pandemic.
Before making changes to its guidance, the CDC had its team of scientists review available data to ensure that there was “an abundance of evidence.”
“For each update to the statement of risks during pregnancy, multiple types of studies and the strength of evidence for each were reviewed,” another CDC spokesperson said. “These reviews of the evidence were accompanied with discussions among subject matter experts both internally and externally with clinical partners for an ultimate determination of risk.”
Dr. Cynthia Gyamfi-Bannerman, a perinatologist and chair of the department of obstetrics, gynecology and reproductive sciences at the University of California, San Diego School of Medicine, shared the daunting task of making vaccine recommendations for pregnant people as part of COVID-19 task forces for two leading organizations, The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine.
In the beginning, she said, the only pregnancy-specific data they had came from a few dozen participants who were inadvertently included after becoming pregnant during the clinical trials and from some pregnant animal data.
“It played out in real time in the COVID pandemic because we see the effects of not including pregnant people in these trials,” Gyamfi-Bannerman said. “We couldn’t make a strong recommendation, so pregnant people were hesitant. I think that directly led to fewer people using the vaccine than we would have wanted.”
At the end of June 2021, the CDC added a general update to its website to reflect the dangers of the delta variant tearing across much of the country. “Getting vaccinated prevents severe illness, hospitalizations, and death,” it wrote. “Unvaccinated people should get vaccinated and continue masking until they are fully vaccinated.”
But it wasn’t until Aug. 11, eight months after the first vaccine was administered, that the CDC issued its formal recommendation that pregnant and breastfeeding people get vaccinated.
“The vaccines are safe and effective,” Walensky said in a statement at the time, “and it has never been more urgent to increase vaccinations as we face the highly transmissible Delta variant and see severe outcomes from COVID-19 among unvaccinated pregnant people.”
August would prove to be the deadliest month for COVID-19-related deaths of pregnant people. The CDC issued an emergency call the next month strongly recommending the vaccine to pregnant people, noting that approximately 97% of pregnant people hospitalized with COVID-19 were unvaccinated. The dangers to symptomatic pregnant people included a 70% increased risk of death, and their developing babies could face a host of perils, including stillbirths.
Researchers have yet to determine exactly why some pregnant people with COVID-19, vaccinated and unvaccinated alike, deliver stillborn babies, while others do not. Attempts to answer that question have been hindered, in part, by incomplete data. The CDC’s statistics on COVID-19-related fetal and maternal deaths are undercounts. The CDC has data on less than 73,000 birth outcomes following a mother’s confirmed COVID-19 diagnosis in 2020 and 2021, of which 579 were pregnancy losses.
That information was sent in by fewer than three dozen health departments, and those estimates don’t include states like Mississippi, which in September reported 72 COVID-19-related stillbirths since the start of the pandemic, nearly double what the state would have expected, according to data from the Mississippi State Department of Health. Preliminary state data shows total stillbirths increased there in 2020 then dipped in 2021, but were still higher than pre-pandemic numbers.
A separate CDC database shows more than 220,000 COVID-19 cases and at least 305 deaths among pregnant people.
“CDC recognizes that pregnant people faced challenging decisions about how to best protect themselves in the setting of uncertainty related to both the infection and the COVID-19 vaccine,” a CDC spokesperson said, adding, “COVID-19 vaccination remains one of the best ways to protect yourself and your family from serious illness from COVID-19.”
Heartbroken and determined, Jaime Butcher has emerged as an unofficial ambassador for the vaccine, posting in online pregnancy and stillbirth forums about the risks of being pregnant and unvaccinated.
No one, she said, told her of the risks. Doctors, the CDC and health officials, she continued, aren’t doing enough to inform people. Even now, well into the pandemic’s third year, the message still isn’t getting through.
“I kept seeing it happening more and more to women and it wasn’t talked about,” she said. “They just say, ‘Oh, get the vaccine,’ which is great, but they don’t talk about what getting the virus can do to pregnant women.”
As a wedding planner, Butcher was surrounded by love. She found it with her husband, then in the daughter growing in her belly, who they named Emily after Butcher’s grandmother.
Butcher suffered five miscarriages before, she said, she opened an email from an in-vitro fertilization clinic confirming her pregnancy in the summer of 2020. She screamed, and her husband rushed to wrap her in a hug.
They waited until she was five months along to announce her pregnancy at Thanksgiving. The next day, Black Friday, they bought a high chair, a tummy time mat and pink onesies.
They were taking precautions, Butcher said, especially since the vaccine wasn’t yet available to her or her husband. But a week later, she woke up with a runny nose, though she didn’t think much of it. Still, she went to the hospital to make sure everything was OK. An ultrasound came back normal.
When her daughter’s kicking slowed the next morning, she called her doctor’s office again. They told her to eat something sweet to get the baby moving. She tried everything she could find: orange juice, Cheerios, Twix, graham crackers, peanut butter and jelly. Nothing worked.
A few hours later, Butcher drove herself to the hospital, where she followed her daughter’s heartbeat on the screen. Steady. Then slow. Then still.
She delivered at 23 weeks. Butcher didn’t know she had COVID-19 until they tested her at the hospital. A lab report later revealed extensive damage to the placenta.
“I was in shock. I was in shock that I lost my daughter, in shock that I had COVID,” Butcher said. “She should be alive, but it’s because of COVID that I lost her.”
A week later, she parked in front of Kohl’s to return the high chair, the clothes still on tiny hangers and the stroller her mom gave her. As she made her way to the register, she saw a baby in an identical stroller. The tears stung all the way down her cheeks.
“You see what you want right in front of you,” she said, “and it’s like, ‘My baby should be here. This shouldn’t have happened.’”
Even before the pandemic, almost a quarter of all stillbirths may have been preventable. The stillbirth crisis has simmered silently in the U.S., claiming the lives of more than 20,000 babies annually. But parents often suffer alone, overwhelmed by grief and guilt.
Butcher, now 45, scheduled her vaccine as soon as she could. Her second dose fell on what was supposed to be Emily’s due date. After getting the shot, she and her husband drove up to Cleveland to visit their daughter’s grave and tell her that her mother got the vaccine in her honor. They let her know how much she was loved and how desperately they wished she was still safe inside her mother’s womb.
They didn’t linger long that spring day. It was a quiet visit. Butcher brought Emily pink flowers, always pink, and said goodbye.
They didn’t know it at the time, but they’d be back in a year to introduce her to her little brother.
Amid the devastation of the pandemic, Heerema-McKenney sees a glimmer of hope. The antibodies from the vaccine have been shown to transfer through the placenta. That immunity in the womb, research shows, reduces the risk of the youngest infants being hospitalized with COVID-19. She continues to encourage pregnant patients to get vaccinated and boosted. If not for them, for their baby.

While 71% of pregnant people were fully vaccinated as of mid-July, a figure not much lower than national vaccination rates for people 18 or older, only around 2% received at least one of their shots while they were pregnant — suggesting that persuading people who are already pregnant to get vaccinated remains a challenge. Research points to a substantial waning in immunity five to eight months after getting the first vaccine, yet only 58% of pregnant people were boosted. Like with booster rates among those who aren’t pregnant, Black and Hispanic people trail behind.
Heerema-McKenney said obesity, high blood pressure, age and diabetes may also increase the risk of stillbirth, but, she said, it appears the strongest risk factor is not being vaccinated.
“We have a set of data saying that the vaccination is safe, and we have a set of data saying that COVID causes an increase in stillbirth. When you’re seeing those two,” she said, “to me it says, ‘Get the vaccine.’”
Another reason for optimism is that the height of SARS-CoV-2 placentitis appears to have coincided with the dominance of the delta variant; Heerema-McKenney said she has not seen a case of COVID-19 directly infiltrating the placenta for months.
Neither has Odronic, who is relieved to get back to her routine work of cancer biopsies after the punishing period last fall when she saw one to two stillbirths a week. Her hospital honored her in November as Physician of the Year for the “tireless leadership she demonstrated during the COVID response,” the first time the award was given to a pathologist.
But, doctors warn, the virus continues to mutate and the risk of stillbirth remains.
“Maybe we’re out of the woods with this, but we just don’t know,” Heerema-McKenney said. “There’s nothing more tragic than seeing a healthy pregnancy end because of something that’s potentially preventable.”
Back in southwest Ohio, doctors released Ginger from the hospital at the end of October, two and a half months after she was admitted. Her oldest daughter, Hailee, who is now 19, got vaccinated shortly after her mother was hospitalized. Ginger said she wanted to get vaccinated when she awoke in the hospital, but she said her doctors told her to wait a bit.
Since then, she said, her fear of the vaccine came flooding back.
At a recent appointment, Ginger listened carefully as her doctor urged her to get vaccinated, which, the doctor said, would be even more important if she were to get pregnant again. Ginger trusted her. “There’s no agenda behind it,” Ginger said. “I will get the vaccine.”
Ginger continues to wrestle with feelings of gratitude and guilt for surviving when her baby did not. In December, the family held a memorial service for the daughter they named Elliotte Jo and called Ellie. Ginger and Kendal were still too grief-stricken to speak, so Hailee and her uncle prepared remarks.
“You have the best dad that I know would have given you everything under the sun and protected you with every ounce of his being,” Hailee said. “And you also have the best mom to guide you through life. Having two older sisters, you would have had the best wardrobe and many visits to Starbucks.”
She breathed laughter into the room, if only briefly.
In June, the family traveled to Florida. As the waves lapped against the shore and the sunrise turned the sky pink, they etched Elliotte’s name in the sand.

Mariam Elba and Gabriel Sandoval contributed research.











