This story discusses pregnancy loss and termination.
Amanda wanted to warn someone. In June 2021, her daughter — the one she and her husband had tried for three years to conceive — had died after only 28 hours. With an underdeveloped nose, she had battled for every breath.
Nobody knew why. Later, an autopsy report revealed their daughter had an extra 13th chromosome. The condition is nearly always fatal.
“But didn’t we test for that?” Amanda recalled asking herself. “That was kind of where the lightbulb clicked.”
Through her doctor, Amanda had gotten a popular prenatal screening from a lab company. It had come back “negative.”
For three major conditions, including the one her baby had, the report gave the impression of near certainty. The likelihood that she would be born without them was “greater than 99%.”
As she recovered from a cesarean section, Amanda found herself facing a long maternity leave without a child. She shut the door to the empty nursery and began spending what seemed like endless hours of that hazy summer learning about the test.
It’s a simple blood draw designed to check for an array of genetic anomalies. But Amanda, a science researcher, read academic articles showing there was a higher risk of inaccurate results than she had realized. (She asked to be identified by only her first name to protect her privacy.)
On Reddit, she found other women reporting problems with the tests, too. She thought Labcorp, the company that made her test, would want to know about the screening that failed her. Maybe by alerting them, she could help other families. Maybe it would help her understand what happened.
“I was trying to gain answers,” said Amanda, now 32. She tried calling Labcorp’s customer service line, but she said she was passed along from one person to another. “It was just a circle,” she remembered.
She phoned Labcorp a second time. The call ended when an employee hung up on her.
Amanda was baffled. Why didn’t the company seem interested in her experience? Why, she wondered, wouldn’t it want to collect this data? Why wasn’t there someone who could answer her questions about how often this happens, and why?
If she had taken any number of other common commercial tests — including certain tests for COVID-19 or, say, pregnancy — the company would have been required to inform the U.S. Food and Drug Administration about reports of so-called adverse events.
But the test Amanda had falls into a regulatory void. No federal agency checks to make sure these prenatal screenings work the way they claim before they’re sold to health care providers. The FDA doesn’t ensure that marketing claims are backed up by evidence before screenings reach patients. And companies aren’t required to publicly report instances of when the tests get it wrong — sometimes catastrophically.
The broader lab testing industry and its lobbyists have successfully fought for years to keep it this way, cowing regulators into staying on the sidelines.
Worried about a growing variety of tests escaping scrutiny, the FDA was on the cusp of stepping in six years ago. But then it backed down.
Peter Lurie, then a top agency official, was at the meetings where the FDA tabled its plans. Not pushing harder, he told ProPublica, “remains one of my greatest regrets.”
The risk of false positives from prenatal screenings, in particular, has been known for years.
In 2014, the New England Center for Investigative Reporting detailed how some companies gave a misleading impression of the precision of the prenatal screenings. Women often didn’t understand they needed diagnostic testing to confirm the results. Some had gotten abortions based on false positive results, the story said. Earlier this year, The New York Times reported how companies sell optional extra screenings that are “usually wrong” when they predict a disorder.
Despite these stories and calls for reform by patient advocates, the government has done little to improve oversight of prenatal screenings. ProPublica set out to examine the forces that led to this inertia and left patients like Amanda feeling misled. Interviews with more than three dozen women revealed ongoing confusion about the screenings — and anger when their reliability proved to be overblown.
“This is a Wild West scenario where everybody is on their own,” said Lawrence Gostin, a Georgetown University law professor specializing in bioethics.
The stakes for families are increasing. Upwards of half of all pregnant people now receive one of these prenatal screenings. And with many states banning abortions or limiting them to early in pregnancies, the need for fast, accurate information has become more urgent.
The FDA itself acknowledges the problem. In correspondence with ProPublica, a spokesperson cited an “outdated policy” regarding the lack of vetting of many lab tests that the agency has “spent the better part of the last two decades trying to address.”
The screening industry, meanwhile, continues to expand, proving lucrative for those who lead it. The chief executive of Natera, which claims about 40% of the market share of prenatal screenings, received a $23 million compensation package last year, the highest of any executive at a publicly traded lab company.
Testing companies told ProPublica that, even without the FDA, there is significant oversight. Labs must abide by state regulations, and another federal agency, the Centers for Medicare and Medicaid Services, is charged with monitoring quality standards. It does not, however, check whether the tests the labs perform are clinically valid.
Companies also said the screenings offer important guidance to expectant families. Echoing others in the field, Labcorp said in a statement that the screenings, when used properly, “provide vital information about the presence of increased risk, but do not provide a definitive diagnosis.” (It declined to discuss the specifics of Amanda’s experience.)
Natera pointed out that its materials tell patients that “this test does not make a final diagnosis.” It reports results as “high-risk” or “low-risk,” not positive or negative.
Companies have stressed that, ultimately, it’s the responsibility of health care providers, who order the tests, to inform patients about the limits of screenings.
For all that, the statistical nuances of the test aren’t easy to parse for patients and even some doctors and nurses. For example, the test for trisomy 13, which doomed Amanda’s baby, is actually less likely to correctly predict the condition than other tests in the standard bundle of screenings offered to every patient.
When ProPublica asked readers to share their experiences with noninvasive prenatal screening tests, often referred to as NIPTs or NIPS, more than a thousand responded. Many said the tests had given them peace of mind. Some said they had provided an early warning about problems.
But others had more questions than answers. None more so than Amanda.
“What are these tests?” she wondered. “And how did mine end up in the margin of error?”
“They Started Using It on Humans, and Then They Went Back and Said, ‘Was Our Test Accurate?’”
Scientists have long tried to find ways to help parents and doctors understand what’s happening inside the womb. Amniocentesis was first used to reveal genetic anomalies in the late 1960s. But it didn’t become more popular until it began to be paired with ultrasound to precisely guide the procedure.
In the 1980s, doctors started using chorionic villus sampling, or CVS, an analysis of placental tissue that offers a diagnosis earlier in pregnancy. But, like amniocentesis, it is an invasive test that involves some risk to the fetus, though experts say it’s exceptionally low.
A breakthrough came in the late 1990s, when a scientist recognized that free-floating placental DNA could be detected in the mother’s blood. This meant that the fetus’s chromosomes could be examined by collecting a blood sample as soon as nine weeks into pregnancy. This also provides an early opportunity to learn the likely fetal sex — a particularly popular feature.
Champions of the new science celebrated the arrival of a simple technique for patients that was particularly precise, at least for some conditions. Many favored it over other noninvasive options. But the industry that developed around NIPT has been marred by controversy from the beginning.
Dr. Ronald Wapner, director of reproductive genetics at Columbia University, described that time as “very chaotic.”
The tests had not been appropriately evaluated in clinical practice, said Wapner, whose research has sometimes been funded by testing companies. Because of this, he said, the industry “had very incomplete data on how well it worked.”
That didn’t stop the excitement. The chief executive of Sequenom, a biotechnology company that planned to release the first NIPT for Down syndrome, championed the company as the “Google of Molecular Diagnostics.” Its stock price soared.
Then, about two months before an expected launch in 2009, Sequenom killed the plan. The company’s research director, it turned out, had manipulated testing data and made misleading claims about how well the screening worked.
The U.S. Securities and Exchange Commission and Federal Bureau of Investigation opened investigations. Top executives were fired, and the research director pleaded guilty to conspiracy to commit securities fraud. Sequenom still managed to commercialize the test in 2011. (Labcorp, which later acquired Sequenom, said it uses a different kind of test.)
Other companies soon debuted their own tests. Still, there was little data on their clinical performance, researchers said.
As Megan Allyse, a bioethicist at the Mayo Clinic, put it, the companies “launched the test, they started using it on humans, and then they went back and said, ‘Was our test accurate?’” She also questioned the lack of attention to the ethics of how tests are presented to patients.
Despite missteps by the industry, the FDA didn’t scrutinize the screenings because they were considered lab-developed tests, which means they are created by the same laboratory that conducts them.
In 1976, Congress revamped oversight over medical devices. Since then, the FDA has effectively exempted such “home-brew” tests from key regulatory requirements. The idea was that when, say, a hospital lab wanted to create a simple test for its own patients, it was spared the time, money and hassle of getting approval from Washington bureaucrats.
Today, lab-developed tests are vastly more numerous and complex. Because they aren’t registered with the federal government, nobody knows how many exist.
The distinction between tests the FDA actively regulates and those they don’t can seem nonsensical. It isn’t based on the complexity of the tests, or how people use them. It’s simply a matter of where the test is made.
The prenatal genetic screening industry took off almost immediately, powered by an army of aggressive sales representatives.
“At the very beginning, obstetricians in practice were being just completely inundated with visits from the sales reps,” said Dr. John Williams, director of reproductive health at Cedars-Sinai in Los Angeles. The push left many OB-GYNs and patients thinking the screenings were accurate enough to substitute for diagnostic tests, such as amniocentesis or CVS.
In some cases, sales tactics escalated into lawbreaking.
Former Sequenom executives who exited during the fraud scandal created a new company that became Progenity, which also offered prenatal screening. Shortly after the company went public in 2020, it finalized a $49 million settlement with federal and state governments, where it admitted to falsifying insurance claims and giving kickbacks to physicians and their staff. According to a legal filing, one sales rep spent $65,658 on meals and alcohol for physicians in one year.
Now called Biora Therapeutics, the company said in a statement it no longer does any laboratory testing, including prenatal screenings.
Industry revenue continues to grow, but some testing companies are still fighting to make a profit, and competition to survive is fierce. “There’s a multibillion-dollar market, and they all want a piece of it,” said a former Progenity sales rep who quit in disgust after five months in 2016.
The rep, who requested anonymity since she continues to work in the field, said she still sees competitors from NIPT companies visiting medical practices “every week, buying breakfast, or dinner, or taking them out for happy hour.”
Over time, companies pointed to new peer-reviewed studies, research the industry itself funded, to earn the confidence of doctors and other stakeholders. They showed that two tests — for Down syndrome and trisomy 18 — often performed better than other screening methods.
This research was valid, said Dr. Mary Norton, a perinatologist and clinical geneticist at UCSF Medical Center’s Prenatal Diagnostic Center. Considered a leading researcher in the field, she authored many of these key industry-funded studies.
But, she said, when research findings were presented publicly, the companies sometimes downplayed “inconvenient truths,” such as the exclusion of inconclusive results from accuracy estimates. Crucial caveats were also glossed over by some companies when they translated research into promotional copy aimed at health care providers and patients. Those materials didn’t always mention the many factors that can limit the performance of the screenings, including high body weight, the rarity of the condition tested and younger maternal age.
Testing companies said they try to help patients understand the screenings through online resources and other materials. Some offer genetic counseling services.
The younger a person is, the lower the test’s positive predictive value — that is, the probability that a positive screening result will turn out to be correct — will be for some conditions. For instance, because Down syndrome is less prevalent in younger people’s pregnancies, a positive screening test is more likely to be a false positive for them.
Kristina was 30 years old in 2016, when her Progenity test came back positive for Down syndrome. She and her husband, who asked not to be fully named to protect their privacy, said they didn’t plan to carry a pregnancy with this condition to term.
But waiting to get an amniocentesis, and then waiting for the results, took five agonizing weeks, she said. It showed her son did not have Down syndrome.
Kristina, who lives in Texas, is still troubled by what she describes as a traumatic experience.
“I researched both late-term abortion providers and cemeteries,” she said. They even picked out a burial place, near their house.
She bought a blue baby blanket she intended to bury the baby’s tiny body in. She still has it. Her son, now 5, sleeps with it every night.


“I Can’t Believe I Didn’t Say More”
As lab-developed tests became a bigger business, moving well past their home-brew origins, regulators looked for a way to assert oversight. In 2014, after years of study and debate, the time seemed right.
The FDA released plans proposing to regulate the tests, prioritizing those used to make major medical decisions. The agency has pointed to NIPTs as one of 20 concerning tests.
But, over the next two years, a coalition of power players urged the FDA to back off. Professional associations issued statements and hosted webinars devoted to the issue. Some created polished websites featuring sample letters to send to Washington.
Academic medical centers and pathology departments joined the fight, too. Scientists from 23 of them put it bluntly in a letter to the Office of Management and Budget: “FDA regulation of LDTs would be contrary to the public health,” it said, using a common acronym for the tests.
“Critical testing would be unavailable in the ‘lag time’ between development of new tests and FDA authorizing them,” the authors of the letter wrote, “and subsequent improvements on existing tests would slow significantly under the rigid, inflexible, and duplicative FDA regulatory scheme.”
This could delay essential care for patients. What’s more, opponents argued, existing lab reviews by the Centers for Medicare and Medicaid Services are sufficiently rigorous. Some have suggested modernizing the CMS review process to improve oversight.
An FDA spokesperson told ProPublica that the agency encountered “continued, negative feedback,” including a 25-page paper written by two legal heavyweights hired by the American Clinical Laboratory Association: Paul Clement, President George W. Bush’s former solicitor general, and Laurence Tribe, law professor at Harvard University.
Clement has reportedly commanded rates of $1,350 per hour. He and Tribe did not respond to ProPublica’s queries about their work.
Their brief argued that the FDA “lacked legal authority” to regulate lab-developed tests because they are properly seen as the practice of medicine: a service, rather than a product.
However, as lawyers representing the American Association of Bioanalysts countered, the FDA would vet tests before they reach the market, not control how doctors use them. The government proposal, they wrote, is “similar to imposing requirements to screen blood or label drugs.”
After the election of President Donald Trump, but before he took office, a handful of FDA officials discussed their battered proposal. It had represented a breakthrough in the decades of excruciating back-and-forth with industry. But now, with an incoming administration bent on deregulation, their efforts seemed futile.
The regulators feared anything they enacted would be undone by Congress — and, under the Congressional Review Act, they might not be able to reissue anything “substantially similar” in the future. So the FDA published a white paper instead, summarizing the issue “for further public discussion.”
After the meeting where officials made this call, Lurie, then the FDA’s associate commissioner, recalled a colleague approaching him: “I can’t believe you didn’t say more.”
“And I was like, ‘Yeah, actually, I can’t believe I didn’t say more either,’” Lurie later told ProPublica. (After leaving the agency, Lurie went on to lead the Center for Science in the Public Interest, a consumer advocacy nonprofit, which has pushed the FDA to finally assert oversight over lab-developed tests.)
Nancy Stade, an attorney and senior policy official who left the FDA in 2015, said the agency often moves slowly as it seeks to get buy-in from industry and professional groups. In her work on regulatory policy, she saw it happen with lab-developed tests.
The agency is “always testing the waters,” she said, “and always coming out with something a little bit softer.”
In 2020, the influential American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine, representing doctors who handle pregnancies, gave the screening industry another huge boost.
In a bulletin updating their advice on the tests, the two groups described growing research on the performance of some of the standard tests and said people have the right to information about their pregnancies, so the tests should be offered to all patients. Previously, they recommended this only for those facing higher risk of genetic anomalies.
The bulletin said the co-authors had disclosed no conflicts of interest. But two of the four co-authors, including Mary Norton, had disclosed in prior publications that test-makers had provided funding for their research. A company had provided a third co-author with laboratory services needed to run tests, according to that researcher, a connection she also disclosed in past papers.
ACOG, in a statement to ProPublica, said the organization “identified no conflicts because research funding is provided to academic institutions with institutional review boards, not to individual investigators.” Two of the three researchers responded to questions from ProPublica and said they maintained independence over their work.
One test-maker, Illumina, celebrated the ACOG guidance in a tweet, saying it “recognizes the superior performance of #NIPT and the benefit it provides expectant families.” Natera’s share prices doubled in five months. UnitedHealthcare, the nation’s largest private insurer and long a target of industry lobbying, told ProPublica it changed its stance to cover screenings for all patients, regardless of risk, because of the recommendation.
In a recent shareholder report, Natera stated that prenatal genetic and carrier screenings “represent the significant majority of our revenues,” which totaled $625.5 million in 2021. The company expects more growth to come.
“The NIPT market is still very underpenetrated, compared to the 4 to 5 million pregnancies in the U.S.,” Natera’s chief executive said on a 2021 earnings call, “so there’s a long way to go.”
But even Norton, who co-authored the ACOG recommendation and favors NIPTs for patients 40 and over, has concerns about screenings becoming widespread among those who are younger. In most cases, she prefers other screening methods that catch the nongenetic problems younger moms are more likely to face. Negative results from an NIPT, she said, can be “falsely reassuring.”
In the years after the FDA set aside its regulatory proposal, the agency has assisted members of Congress on a proposed legislative solution. That effort, dubbed the VALID Act, aims to end any debate over the agency’s authority over lab-developed tests. An FDA press officer said the legislation would ensure the prenatal screening tests and others are “accurate and reliable.”
But, as in the past, intense lobbying followed the proposal. The VALID Act was a rider to a funding reauthorization bill, but in September the House and Senate agreed to remove it. Advocates now hope to attach it to proposed end-of-year legislation.
Meanwhile, earlier this year, four months after the New York Times story on the usefulness of some screenings, the FDA took a step toward more public awareness about prenatal genetic screening. It issued its first safety communication on them, noting the potential for false results.
It cautioned patients about making “critical health care decisions based on results from these screening tests alone.”
Cara Tenenbaum, a former FDA policy advisor, was pleased to see the statement. Still, she said, it was long overdue.
“This has been known — known, or should have been known — for 10 years,” she said.
“It Had Me So Messed Up”

With the demise of Roe v. Wade, restrictive and ever-changing abortion laws can pressure people to act quickly with limited information, heightening the stakes of prenatal screening.
Julia, a mom from Mississippi’s Gulf Coast, knows what it’s like to face harrowing consequences while navigating state-imposed time limits — and doing so with little guidance. Last fall, she was pregnant with her fourth child when, she said, a nurse practitioner suggested prenatal genetic screening.
At 33, Julia had no risk factors. Her previous pregnancies hadn’t been screened with an NIPT. But with three sons and 18 nephews, she and her husband were curious about the baby’s sex. And the screening seemed like it had no downside.
Julia figured it would only be offered if it was reliable, so her nurse practitioner ordered her both the basic bundle of screenings and the extra tests. (The medical practice didn’t respond to interview requests. Julia is a family nickname that’s used here to protect her privacy.)
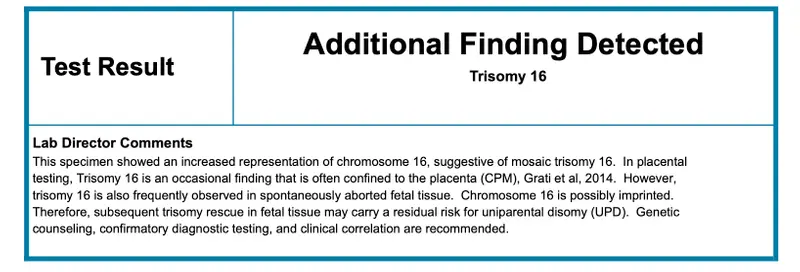
The screenings showed the baby was a girl — but the extra tests also detected trisomy 16, a condition caused by an extra chromosome that is so rare, the nurse didn’t know what it was, Julia recalled.
The nurse borrowed Julia’s phone, using it to search online and read aloud what she found. Julia was stunned to hear trisomy 16 was incompatible with life.
“I was utterly devastated,” she said. “I made it out of my doctor’s office but completely broke down in the car.”
But ACOG does not recommend the trisomy 16 screening, saying “its accuracy with regard to detection and the false-positive rate is not established.” Julia wasn’t informed of this, she said, and she’s not sure if her health care providers knew it either.

The lab report recommended diagnostic testing to confirm the results, but time was short. She had her amniocentesis at 17 weeks. It could take up to four more weeks to receive results.
That would be too late for a legal abortion in Mississippi. So she made an appointment for one in Florida, where the cutoff was 24 weeks. (It’s now 15 weeks in Florida, while Mississippi went from 15 weeks for legal procedures to a ban on nearly all abortions.)
The wait was excruciating. Julia was driving twice a week to New Orleans for specialized care. With work and child care, it was too hard. She quit the teaching job she loved.
One winter night, she felt the fetus move for the first time — ordinarily a milestone, but now, facing a fatal prognosis, she didn’t want to get attached. “It had me so messed up,” she said.
On the way to the amniocentesis, Julia and her husband chose a name. Drawing from a language conjured by J.R.R. Tolkien in the fantasy novels they love, it means “hope.”
More than halfway through her pregnancy, the amnio results arrived. The prenatal screening had given a false positive. The baby would be fine. In May, Julia gave birth to a healthy daughter.
Julia and her husband are upset about the needless anguish brought on by the screening. “They like to have it both ways,” said Julia’s husband. “They say they are 99% accurate, but when there's a false positive, they say, ‘Well, we’re not diagnostic.’”
Believing the prenatal screening was likely accurate, they had seriously considered canceling the amniocentesis, saving their limited funds for an abortion in Florida, hundreds of miles away.

Their dilemma points to a longtime concern: ending pregnancies based on false positives. The FDA cited it as a risk as far back as 2015. Now, those with positive results are facing an even tighter time crunch. They must consider whether waiting for a definitive test, and possibly traveling to another state for an abortion later in pregnancy, is worth it.
In their promotional material, some companies not only sidestep the variability of the standard tests, they fail to distinguish them from the least reliable ones — those for exceptionally rare conditions. They tout the extra screenings as “premium,” “plus” or “advanced” options.
“Going to greater lengths for the answers that matter most,” says a brochure aimed at health care providers from test-maker Illumina. Elsewhere it states that the “expanded” panel of tests provides “confident results” and “the additional insights you need.”
But the companies themselves know the accuracy of some of their tests has yet to be established in the research. Natera acknowledged in a recent shareholder report that many insurers won’t pay for screenings for missing chromosomal fragments, known as microdeletions, in part because there isn’t enough published data behind them.
The company, responding to ProPublica, stressed the quality of the data over the quantity, saying the research so far has been favorable. “Natera’s microdeletion testing was thoroughly validated with results published in peer-reviewed publications,” it said in a statement.
Natera pointed to a recent study that looked at DiGeorge syndrome, one of several chromosomal anomalies it checks for with its microdeletion screenings. Researchers found the positive predictive value of the test to be 52.6%, meaning that nearly half of positive results are false positives. (For many patients, PPVs for more common conditions can exceed 90%.)
Natera said the performance of the diGeorge syndrome test “is excellent and not considered a low PPV,” due to the condition being extremely rare.
Companies also play up the danger of diagnostic tests like amnio. They “can cause miscarriages,” warns the marketing from Labcorp, which made Amanda’s screening, while its test “does not cause miscarriages.” But medical experts emphasize that diagnostic tests, such as amniocentesis, are more accurate and, in fact, carry little risk to the pregnancy.
Labcorp, in a statement, said the company “acknowledges the well-documented risk associated with amniocentesis and CVS in our literature. It is the patient’s prerogative to decide which risks they are willing or unwilling to take.”
Marketing claims also sometimes skate over the nuances in the guidance from the leading professional societies. On a webpage targeting health care providers, for example, a Labcorp chart said groups such as ACOG “endorse and/or recognize” prenatal screenings as an option for all pregnancies. But the chart listed screenings ACOG does not recommend, including trisomy 16.
When asked about it, Labcorp said in a statement that ACOG “endorses NIPS for all pregnancies.” In fact, the guidance is not so sweeping. It says only that the basic bundle of tests should be offered to all, alongside other screening options. It explicitly advises providers to not offer patients the extra tests.
Soon after ProPublica’s query, the Labcorp webpage was updated to remove any mention of the professional societies.
Patients say they often don’t know where to turn for informed and unbiased information. That’s why the r/NIPT Reddit page became such a robust community. Facing difficult news, Julia turned to it for counsel from other prospective parents. Kristina in Texas found the same community. Amanda, too.
“The Margin of Error Is a Human Life”
On a warm and cloudy day this past June, on what would have been their daughter’s first birthday, Amanda and her husband visited her grave. They brought a unicorn balloon and vanilla cake, which they ate nearby on the grass. Her husband read a poem.
To them, their baby had been perfect. She had fingers and toes. A thatch of dark hair. While in intensive care, peering up at her parents, she grabbed for her mother’s hand.
Had her condition been known, they would’ve spared her futile medical interventions, as doctors tried to save her life. Their family priest would have been able to baptize her. As it was, they never got to hold their child while she was alive.
These days, when Amanda and her husband say grace before dinner, they give thanks for the 28 hours of their daughter’s life.
They’re also thinking about making comfort boxes the hospital could give to other parents who lose a child. It might include books on grief. Softer tissues. Something that says, as Amanda puts it, “This is to help you get through.”
Amid their grief, they had a prayer answered: Amanda is pregnant again.
It’s frightening to go through this again. She barely sleeps the night before visiting the doctor. It feels like she never stopped being pregnant. It will feel that way, she said, until she brings a baby home — one who lives past the first two nights.
Amanda planned to get another genetic screening test. At first she couldn’t bear it, wasn’t sure she could trust it. “The margin of error is a human life,” Amanda said.
The 10-week appointment passed. Then the 12-week appointment. After her 13th week, she took the plunge. The test she was given was from Labcorp.
Around this time, more than a year after Amanda had desperately tried to alert the company about what had happened to her and her first baby, she finally heard back. Labcorp’s vice president of genetic counseling and services reached out — after ProPublica contacted the company and shared Amanda’s story.
The executive would only speak to Amanda without a reporter present.
Amanda said that during the call, the executive told her that prenatal genetic tests are evolving, and doctors should be clear about what the screenings can and cannot do. By the end of the conversation, the executive offered Amanda her cell number.
Amanda said she appreciated the call. “I feel better. I feel like I got something.”
The same day, her screening results came back. They were negative.










