Join us for an upcoming live virtual event, “Post-Roe: Today’s Abortion Landscape.”
This story graphically describes serious complications in pregnancies and births, and it mentions suicide.
One day late last summer, Dr. Barry Grimm called a fellow obstetrician at Vanderbilt University Medical Center to consult about a patient who was 10 weeks pregnant. Her embryo had become implanted in scar tissue from a recent cesarean section, and she was in serious danger. At any moment, the pregnancy could rupture, blowing open her uterus.
Dr. Mack Goldberg, who was trained in abortion care for life-threatening pregnancy complications, pulled up the patient’s charts. He did not like the look of them. The muscle separating her pregnancy from her bladder was as thin as tissue paper; her placenta threatened to eventually invade her organs like a tumor. Even with the best medical care in the world, some patients bleed out in less than 10 minutes on the operating table. Goldberg had seen it happen.
Mayron Michelle Hollis stood to lose her bladder, her uterus and her life. She was desperate to end the pregnancy. On the phone, the two doctors agreed this was the best path forward, guided by recommendations from the Society for Maternal-Fetal Medicine, an association of 5,500 experts on high-risk pregnancy. The longer they waited, the more complicated the procedure would be.
But it was Aug. 24, and performing an abortion was hours away from becoming a felony in Tennessee. There were no explicit exceptions. Prosecutors could choose to charge any doctor who terminated any pregnancy with a crime punishable by up to 15 years in prison. If charged, the doctor would have the burden of proving in front of a judge or jury that the procedure was necessary to save the patient’s life, similar to claiming self-defense in a homicide case.
The doctors didn’t know where to turn to for guidance. There was no institutional process to help them make a final call. Hospitals have malpractice lawyers but do not typically employ criminal lawyers. Even local criminal lawyers weren’t sure what to say — they had no precedent to draw on, and the attorney general and the governor weren’t issuing any clarifications. Under the law, it was possible a prosecutor could argue Hollis’ case wasn’t an immediate emergency, just a potential risk in the future.
Goldberg was only a month into his first job as a full-fledged staff doctor, launching his career in one of the most hostile states for reproductive health care in America, yet he was confident he could stand in a courtroom and attest that Hollis’ condition was life-threatening. But to perform an abortion safely, he would need a team of other providers to agree to take on the same legal risks. Hollis wanted to keep her uterus so she could one day get pregnant again. That made the operation more complicated, because a pregnant uterus draws extra blood to it, increasing the risk of hemorrhage.
Goldberg spent the next two days trying to rally support from his colleagues for a procedure that would previously have been routine.
Vanderbilt declined to comment for this article, but Hollis’ doctors spoke to ProPublica in their personal capacity, with her permission, risking backlash in order to give the public a rare view into the dangers created when lawmakers interfere with high-stakes medical care.
First, Goldberg and a colleague tried the interventional radiology department. To lower Hollis’ chance of bleeding, Goldberg wanted doctors to insert a special gel into the artery that supplied blood to her uterus to reduce its flow. But that department’s leadership didn’t feel comfortable participating.
Next, they approached a maternal-fetal medicine specialist who a week earlier had said he would be able to provide an injection to stop the fetus from growing and decrease blood flow. But once the law went into effect, that specialist grew uneasy, he told ProPublica. He asked that his name not be used because of the sensitivity of the issue.
The specialist would have to do the procedure in a room of nurses and scrub techs with an ultrasound image projected on the wall — all potential evidence that could be used against him in a trial. He thought about his family, what it would mean to go to prison. “I’m so disappointed in myself,” he told Goldberg and his colleague as he refused to participate.
That night, Goldberg went home and buried his face into the soft fur of his 100-pound Bernedoodle dog, Louie. He believed strongly that knowing how to perform an abortion was a necessary part of health care; he’d spent two years training in Pittsburgh to have the skills to help people like Hollis. Now he felt like everyone was leaving him alone with the responsibility. He worried about being able to manage that massive bleed alone.
He felt sick when he told Grimm his decision: “It’s too dangerous,” he said.

Grimm felt a mix of anger, fear and sadness burning beneath his ribs. He could scarcely believe the situation. Raised Christian in the deep South, he had never agreed with abortion as a moral choice. But as an OB-GYN whose patient was in mortal peril, he couldn’t begin to comprehend what politicians were thinking. He had told Hollis an abortion ban was coming, but had thought there would be an exception for cases like hers that came with high risks.
He knew Hollis would have difficulty traveling. It began to sink in: The families who would most starkly bear the consequences of the law would be those with little means, whose fragile stability could be disrupted by any unexpected hurdle.
He collected himself as he dialed Hollis. It was Aug. 26, the day after the ban went into effect.
It was also Hollis’ 32nd birthday. She was at her job as an insulator apprentice, monitoring her co-workers as they wrapped rolls of fiberglass around pipes, when she saw Grimm’s name flash on her phone. She headed outside, her long hair coiled under a hard hat, her stomach churning.
The past month had been a dizzying, sickening whirlwind of thrill, then worry, then stubborn hope, then all-consuming terror. She didn’t want to lose her pregnancy, but she didn’t want to die. She had anguished over the decision, prayed about it with her husband, gotten a second opinion and gone around and around with Grimm.
Now, as she stepped outside to take the call, all she wanted to hear was her doctor’s usual calm reassurance and the plan for her care.
But Grimm’s voice was heavy as he began:
“I’m so, so sorry.”


Few Tennessee lawmakers stopped to consider the ramifications when they gathered in 2019 to pass what would wind up being one of the nation’s most severe abortion bans.
It was a trigger law, just words on paper as long as federal abortion rights granted by a 1973 Supreme Court ruling remained in place. “It wasn’t like Roe v. Wade was on the verge of being overturned,” said state Sen. Richard Briggs, a heart surgeon who co-sponsored the bill. “It was theoretical at that point.”
To many, the ban seemed like a publicity stunt. It didn’t even get much pushback from doctors or abortion-rights advocates.
But the influential anti-abortion group National Right to Life was following a strategy.
For decades, the group’s leaders have written and lobbied for model legislation aimed at injecting their particular vision of morality into abortion regulations around the country. In many conservative states, they exert a stranglehold on politics, publishing annual scorecards to track lawmakers’ votes on anti-abortion legislation and funding primary challengers against candidates they don’t consider committed enough.
Invigorated by President Trump’s conservative Supreme Court nominations starting in 2018, they pushed so-called “trigger bans,” designed to go into effect in a future where Roe was overturned. It’s an approach Bob Ramsey, a Republican legislator in Tennessee at the time, likened to throwing spaghetti at the wall “to see what sticks.”
Republican lawmakers knew that voting against the abortion ban bill could spell political peril.
“Unfortunately, it's all about the next election,” Ramsey said. “We didn’t get together and debate the morality of pro-choice or the confusion for medical providers. It was pretty much a foregone conclusion.” In the end, he abstained, and lost his next primary to an opponent who castigated him for not being anti-abortion enough.
But the law sailed through without Ramsey, on party lines.

The Supreme Court’s decision came on June 24, 2022. Tennessee’s abortion ban kicked in two months later. Overnight, procedures that had not been considered “abortion” by many, but simply part of reproductive health care, were a crime. That included offering dilation and evacuation procedures to patients whose water broke too early or who started bleeding heavily in their first trimester. Terminating dangerous pregnancies that never result in a viable birth, like those that settle inside a fallopian tube or develop into a tumor, was also technically an abortion. Each case now presents doctors with an ethical dilemma: Provide the patient the standard of care accepted by the medical community and face a potential felony charge, or try to comply with the broadest interpretation of the law and risk a malpractice case.
National Right to Life considers Tennessee’s abortion ban its “strongest” law, and the group’s Tennessee lobbyist has said the law should only permit abortions that are urgently necessary, such as for someone bleeding out, and not allow those “to prevent a future medical emergency.”
Gov. Bill Lee has defended the law as providing “maximum protection possible for both mother and child.” But some who voted in favor of the bill have since acknowledged they didn’t read it closely or understand how completely it tied the hands of doctors. Briggs, the bill’s co-sponsor, has advocated for changes and lost the endorsement of Tennessee Right to Life.
Tennessee’s ban and others triggered across the country are already unleashing havoc. The uncertainty over how the vague standards will be treated in the courts has created a chilling effect on patient care, doctors and other experts say. Though most bans contain exceptions for abortions necessary to prevent a patient’s death or “a serious risk of the substantial and irreversible impairment of a major bodily function,” data suggests few people have been able to access abortions under those exceptions.
ProPublica reviewed news articles, medical journal studies and lawsuits and found at least 70 examples across 12 states of women with pregnancy complications who were denied abortion care or had the treatment delayed since Roe was overturned. Doctors say the true number is much higher.
Some of the women reported being forced to wait until they were septic or had filled diapers with blood before getting help for their imminent miscarriages. Others were made to continue high-risk pregnancies and give birth to babies that had virtually no chance of survival. Some pregnant patients rushed across state lines to get treated for a condition that was rapidly deteriorating.
Dr. Leilah Zahedi-Spung, a maternal-fetal specialist who left Tennessee in January because of the trigger ban, said that after the law went into effect, she referred an average of three to four patients out of state every week for abortion care to address high-risk conditions she could no longer help with.
But, she said, not everyone has the resources or ability to leave the state for an abortion.

Raised in the depths of Tennessee’s opioid epidemic in a family haunted by addiction, Hollis’ earliest memory is of clutching her baby brother when she was 5 years old, as her alcoholic father flipped tables. When she was 9, she said, her mother’s boyfriend gave her drugs and read her the Bible before he molested her. By 12, she was living with a teenage boyfriend and babysitting his brothers in exchange for hydrocodone pills.
At 21, Hollis began having children: first a son and then two daughters. At 27, when she had her third child, she was trying to stay sober. But the father of that child, Chris Hollis, showed up to the hospital high on opioids. The Department of Children’s Services drug tested him and took custody of all of Hollis’ children.
If her life with her kids had been chaotic, hustling to survive in the pill mill economy and dealing with multiple arrests, her life without them was a black hole of shame and self-hatred. She gave in to drugs and fights and ended up living on the street; one day, in September 2019, she landed in the hospital after an attempted suicide. Three days later, she was a passenger in a car crash that killed a close friend. It was at that moment that she decided she wanted to live. She went from the hospital to rehab.
When Grimm met her in 2021, at a clinic for mothers with opioid use disorder, she was pregnant with her fourth child and sober. He believed Hollis could stay that way; she was sufficiently exhausted by her cycles of addiction. He often used her progress forging a new path for her family to inspire other mothers in the program. He liked her fast-talking boldness and how she owned her past. She liked the way he listened and didn’t judge.
After baby Zooey arrived in February 2022, it seemed to Hollis like life was finally gathering momentum. She had reconnected with Chris Hollis, who she first befriended working at Wendy’s as a teenager. She had always known he held a flame for her, from the time he offered to take her duties cleaning the Frosty machine. Over the years they broke up and reconnected multiple times.
Now both in recovery, they had gotten married, rented a house in Clarksville, a small town near a military base, and joined a church. Together, they ran a small vinyl siding business. Hollis managed the accounting and worked a factory job for extra income. She began to study for her peer recovery specialist certification, imagining a day when she would help other mothers climb out of addiction. She hoped to save enough money to buy a house and eventually pay lawyers to get her other children back.
But three months after Zooey’s birth, Hollis faced a major setback.
Someone accused her of leaving her daughter unsupervised in a car outside a vape shop, records show. Hollis disputed it, but the Department of Children’s Services put Zooey in the custody of her cousin while they investigated the allegation of child endangerment. Hollis and her husband moved out so the cousin could live at their family home.

Then, in July, Hollis was shocked to learn she was pregnant again; she’d just begun taking birth control pills, but it might have been too recent for them to be effective. Her first call was to Grimm, who worried that a pregnancy this soon, on top of four previous C-sections, put her at risk of developing a cesarean scar ectopic pregnancy. By Hollis’ eight-week ultrasound in early August, Grimm’s worst fears were confirmed.
Her life was at risk, he told her. Her pregnancy could rupture and cause a hemorrhage in the first trimester. It was almost certain to eventually develop into a life-threatening placenta disorder. There was little data to predict whether the baby would make it. If it survived, it was sure to be born extremely early, spend months in critical care and face developmental challenges. He offered to schedule an abortion for two days later. If they moved quickly, the procedure would be relatively straightforward. But Hollis needed time to think.
She’d felt a faint thrill when she learned about the tiny life inside of her. Building a family with her husband in their fragile new stability had felt like a chance to redeem herself. Abortion went against her beliefs. What if this was her last chance to have another child?
Grimm gave her his cell phone number. “Want you to know this is so difficult,” he texted. “With you, no matter what you decide.”
It was the second opinion, two weeks later, that convinced her. Doctors at another hospital confirmed her condition was, indeed, life-threatening and already worsening. One of the only places in Tennessee equipped to handle a pregnancy as complicated as hers was Vanderbilt.
“Honey,” her husband told her, “I can’t lose you.”

On Aug. 24, about two weeks after learning the diagnosis, she messaged her doctor:
“Dr. Grimm, me and my husband need to talk to you. We have really thought about everything and we need you to call us.”
But two days later, Hollis paced outside her workplace listening to Grimm break the news that the other doctors had backed out “due to the current legal climate.”
The only thought Hollis could muster was no. No no no no no. This could not be happening. Not now.
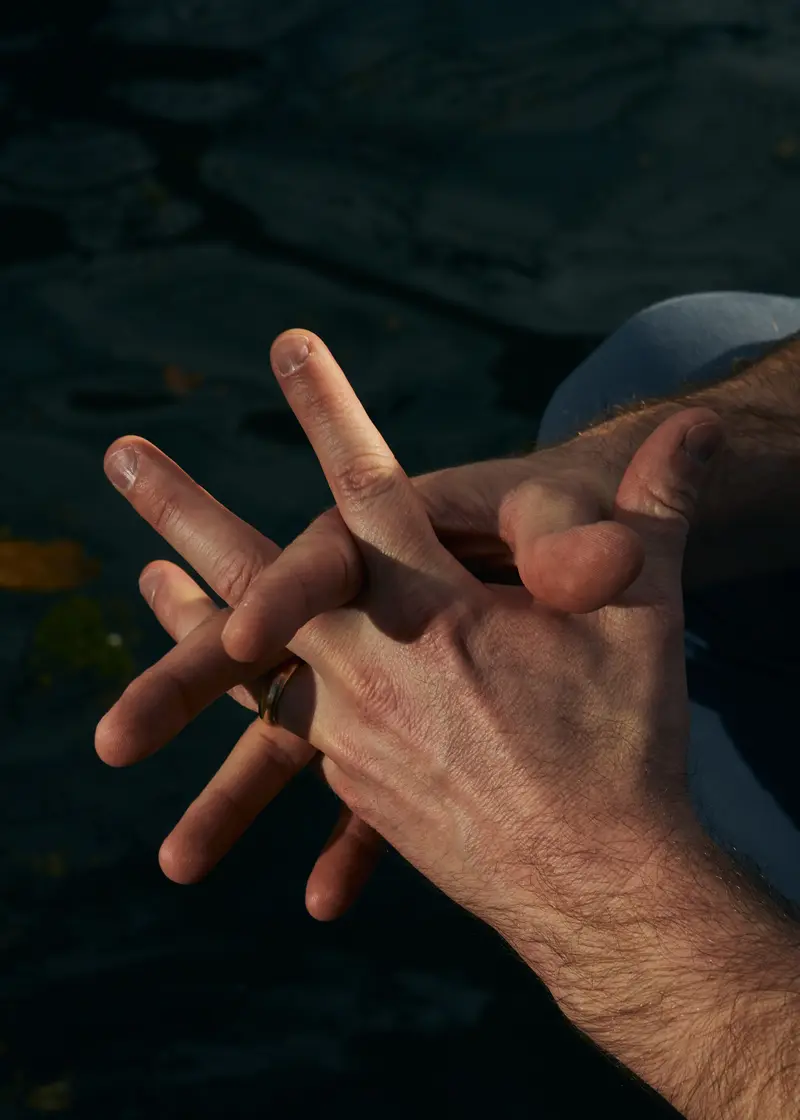
She squeezed her thumb in her fist as Grimm explained that Vanderbilt couldn’t offer an abortion that would try to preserve her uterus — only a hysterectomy that would end the pregnancy and extinguish any chances she could ever get pregnant again. Grimm told ProPublica it was his understanding that ending the pregnancy this way would comply with the law’s provision for avoiding irreversible impairment to a major bodily function. Other doctors involved in her care confirmed they felt their only option for providing an abortion was to sterilize her.
Grimm told Hollis they could help her arrange to travel out of state, where doctors could perform an abortion and possibly save her uterus. Each day that passed would make that more difficult. Going to Pittsburgh, where Goldberg had connections, was her best option, but would require days of travel to complete paperwork and comply with Pennsylvania’s state-mandated waiting period.
Hollis felt trapped in a different kind of risk calculation: At the same time the state was trying to force her to keep her pregnancy, it was also threatening to take away her daughter.
Already, she and her husband hovered over their phones in case Zooey’s case workers needed their attention. She worried she might be accused of abandonment if she left. She also feared losing her job. Her bosses at the factory had laid her off for “personal reasons” after learning she was pregnant for a second time in less than a year, she said. She had just started a new job and relied on it to help pay two rents and $9,000 for a lawyer to fight to keep Zooey. She didn’t know where she would get money for a sudden trip anyway.
She hung up with Grimm, went back inside and cried for the rest of her shift.
As the months passed, Tennessee’s medical community grappled with the real world implications of the new legal landscape.
Vanderbilt, the largest hospital in the state and a private institution, promised its doctors it would pay to defend against any criminal charges and was able to resume offering limited medically indicated abortion care, according to multiple doctors. Vanderbilt declined to comment.
Goldberg and his colleagues’ approach evolved. They began to admit nearly every patient and make each specialist individually assess them. It was costly and time-consuming, but Goldberg believed it made a difference for medical providers to have to look a patient in the eye before refusing to participate in their care. If they agreed an abortion was appropriate, he wrote up long defenses of the patient’s condition and had three other doctors sign off.
Still, almost weekly, Goldberg found himself having to turn away patients he believed should qualify for medically indicated abortion care. He and his colleagues also noticed that doctors at smaller hospitals, who had far less support, seemed to be treating complex cases as hot potatoes and sending them to Vanderbilt. That delayed care for patients. Goldberg worried about those who might not get transferred in time.
ProPublica spoke with 20 Tennessee medical providers about life under the ban, on condition of anonymity because they feared professional and personal repercussions; some said that they had witnessed a new trepidation in their ranks. “I’ve seen colleagues delay or sit on assessing the clinical data longer when they know the diagnosis is probably ectopic,” one said, referring to pregnancies that implant outside the uterine cavity, which are always life-threatening. “People were like, 'I don’t want to be involved because I don’t want to go to prison,'” said another. “It’s crazy — even assessing the patient or having a role in their care makes people scared.”
Meanwhile, Goldberg’s wife, a therapist who asked that her name not be published to protect their family’s privacy, was hearing from a number of pregnant patients who had bled for weeks, but didn’t understand why. Their providers hadn’t mentioned the word “miscarriage” or offered dilation and evacuation procedures. Instead they were told, “Let your body do what it’s going to do.”
Once the ban went into effect, Hollis felt doctors in Tennessee were afraid to touch her. A few days after her conversation with Grimm, overwhelmed, she texted him: “Schedule a hysterectomy.” He asked her to call him, but before she could, she began to feel an intense pain that made her double over.
She went to an emergency room near her home, but left after an hour without being seen. She drove to Vanderbilt and told workers she was at risk for a placenta disorder, the complication Grimm had told her she was showing signs of developing, hoping to get seen more urgently. “Nobody even looked at me after that,” she said. She remembered waiting for hours in triage, crying and incontinent, until she gave up and headed to a third hospital, which gave her antibiotics for a urinary tract infection. Doctors had spent weeks explaining her condition was life-threatening; she didn’t understand how she could be left to sit in a waiting room.
She never brought up the hysterectomy again. “I thought the law meant I couldn’t have one,” she said. Grimm didn’t follow up about the text and said he always remembered Hollis emphatically saying she wanted to try to preserve her fertility.
As friends and coworkers began to ask her about her visible pregnancy, Hollis acted excited. But there was nothing happy about the experience. She constantly worried about what her husband and Zooey would do if she died, and called up the Social Security Administration and her union to find out what kind of survivor benefits existed. She moved through her days trying to pretend she wasn’t pregnant. It was the only way to keep the overwhelming fear at bay and continue working. Then, in mid-November, her employer laid her off, saying it couldn’t accommodate the work restrictions required by her doctor.
At regular appointments, Grimm watched in horror as her placenta began to bulge and threaten her bladder, an expected consequence of a cesarean scar ectopic pregnancy. She was exhibiting all the signs of developing placenta percreta, the worst form of a placenta disorder, a condition that makes high-risk specialists shudder. Delivery requires massive blood transfusions, often necessitates removal of the bladder and carries a 7% chance of death.
Grimm didn’t know what to do for Hollis other than to lower his boundaries and try to support her whenever she needed him. Her texts came at all hours — about her problems sleeping, her concerns about paying rent, her worries about the baby’s movement and the pains she felt. She had not been at her company long enough to qualify for disability leave and begged him to help her appeal: “I’m not sure what else to do, I am running out of time and I’m scared.”
In the end, he couldn’t offer much more than directing her to social workers and sharing earnest platitudes: “You’re the bravest person I know,” he told her.
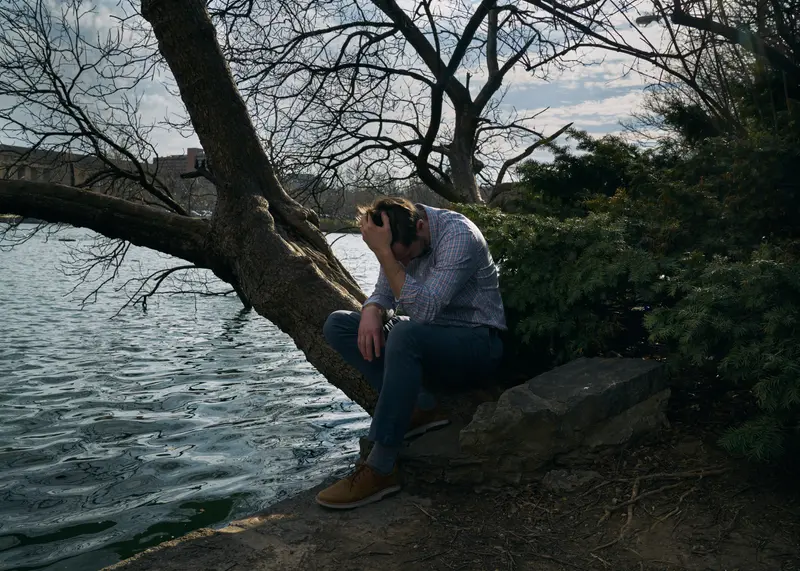
Grimm’s wife noticed the weight he carried home. He found it difficult to be present, zoning out at his kids’ sports games and leaving the dinner table to respond to calls. The culture of medicine assumed that doctors always had the answers and could never make mistakes. But Grimm felt helpless and wrestled with feelings of shame. In his darkest moments, he wondered if a different doctor would have somehow done better by her.
Grimm had always stayed out of politics. But in conversations with family and friends, he began to share more about his work for the first time. Many in his circle abhorred abortion and thought they supported the idea of a ban. He tried to explain that it was more complex. “If this was your wife or my wife in these really intense situations, they'd be fine, because you have the resources,” he told them. “But some people don’t. And they’re going to be forced into these impossible situations where they could die.”
He knew of doctors who had left the profession after losing a pregnant patient. He wondered if this would be his quitting moment.
On Dec. 8, Hollis started bleeding. She was nearly 26 weeks pregnant. She insisted on driving herself to Vanderbilt, an hour away from her home; her husband joined her in the passenger seat and panicked when she started to pass out. They called 911, and an ambulance drove her the rest of the way.
Dr. Sarah Osmundson, a maternal-fetal medicine specialist, was on call that day. She worked exclusively with the most difficult pregnancies, where every decision was a calculation between a pregnant patient’s health and the chances of delivering a healthy baby. It was her job to help patients make an informed decision. Over the years, she said, she had seen some women choose to accept the risks of a dangerous diagnosis and die as a result. But since the law went into effect, patients were arriving at her office asking why they were being counseled all: “It doesn’t matter,” they told her. “I don’t have a choice.”
She could tell Hollis was scared; she felt afraid as well. While she and her colleagues worked to help patients go out of state, she knew of some with cancer, heart conditions, preeclampsia or fatal fetal anomalies who felt forced to continue their pregnancies under the law. She feared it was only a matter of time until one of them died from the complications. She hoped it would not be Hollis.
She wanted Hollis to stay in the hospital for monitoring, but Hollis begged to go home. Zooey’s child welfare case had been closed in October, and she didn’t want to be away from her baby any longer than necessary. She had Christmas presents to wrap, bills to pay and a nursery to set up before her new baby arrived. On top of everything, her fridge was empty and her washer and dryer had stopped working.
Osmundson gave Hollis her phone number, and the hospital released her after three days, planning for her to return in two weeks, when her pregnancy had reached seven months.

But less than two days later, in the early morning hours of Dec. 13, Hollis’ husband woke to screaming. He ran to her and slipped in her blood, which was pooling on the ground. Hollis had bled through her pants, soaking her socks and the rug by the front door. She and her husband texted photos to Osmundson, who became convinced an emergency cesarean needed to happen as soon as possible.
As soon as Grimm’s phone rang, he was wide awake. He lay in bed in the dark, calling the hospital and refreshing his phone for updates. At any moment, he knew, Hollis could bleed to death.
Hollis’ husband called an ambulance, and they took her to a local hospital to be stabilized and airlifted. But bad weather meant the helicopter couldn’t fly. Finally, two hours later, they returned to the ambulance, which drove her to Vanderbilt.
Hollis was relieved to see Grimm waiting in his scrubs. He held her hand as they wheeled her into the operating room, which was filled with a surgery team of nearly 20 doctors. She looked pale and petrified. “We will be right there with you the whole time,” he told her.
To Hollis, the doctors around her looked as scared as she was. The anesthesiologist told Hollis to count backwards from 10, but instead she prayed.
Once Hollis was under, Grimm helped make the incision. Typically, patients emerge from a C-section with a small, horizontal cut below their bikini line. But this delivery called for a vertical gash that stretched up past her navel so doctors could have full exposure to her uterus. It allowed them to see where the bleeding was coming from and gave them the best chance to control it.
Careful not to disrupt the placenta, which was attached to the bladder and ballooning outward, Grimm gently removed a baby girl. She emerged weighing one pound and 15 ounces, limp and unable to breathe on her own. Doctors dried and intubated her, wrapped her and placed her under a radiant warmer to try to keep her organs from shutting down. No one knew if she would survive.
Then, Dr. Marta Crispens, a gynecological oncologist trained to deal with big tumors, began work on removing the uterus. The placenta started gushing blood again. This was what made the condition so frightening: There was no predicting the level of bleeding and whether it could be contained in time. The intensity in the room ratcheted up. It seemed to Grimm like hours passed as he helped Crispens stanch the bleeding, though it was only minutes.
Hollis was given a blood transfusion. Finally, the operation ended. Hollis and her daughter had made it through alive.
As the doctors cleaned up, there were the usual back pats and shared congratulations between a team that had united to make it through a life-saving surgery. But they could all recall similar cases where things didn’t end as well.
“I’m glad she’s OK,” Osmundson recalled saying in the moment. “But it’s a tragedy that this happened — this is not a win.”
Crispens felt everyone in the room was traumatized. “This is going to drive people out of the medical profession,” she thought. “We took an oath — we have to be able to take care of these women before they get to this point.”
Grimm left the room, peeled off his scrubs and wept.
When Hollis awoke from surgery, he was holding her hand.
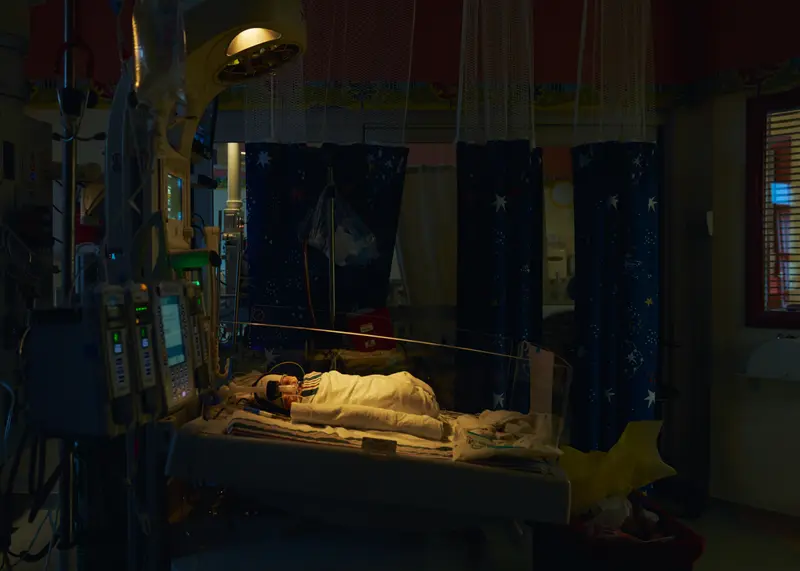
Baby Elayna spent the first week of her life in the neonatal intensive care unit, enclosed in a plastic crib that resembled an aquarium. Nurses bustled in and out to the sound of beeping that monitored the baby’s fluctuating breathing and heart rates.



Her skin was pink and translucent, wires and patches poked out from all over her body, and her tiny face was covered with a breathing machine. Nurses told Hollis that Elayna was too fragile to be held. Hollis could only stick a latex-gloved hand through a hole in the crib to feel Elayna’s penny-sized grip on the tip of her finger. Over that first week, doctors monitored Elayna’s brain for bleeding and poured a protein into her breathing tube to help her lungs open and close.
Though Elayna's survival seemed assured, she faced significant hurdles. About 80% to 90% of babies born at 26 weeks survive. Of those, about 40% end up with brain injuries. Over the first two years of life, 12% may develop cerebral palsy, and some have vision, hearing and intellectual development issues. Elayna would be particularly vulnerable to flu and other respiratory illnesses. About half of babies born prematurely get readmitted to the hospital within the first two years. The cost of her care, which included more than two months in the NICU, would come out of the taxpayer-funded state Medicaid program.
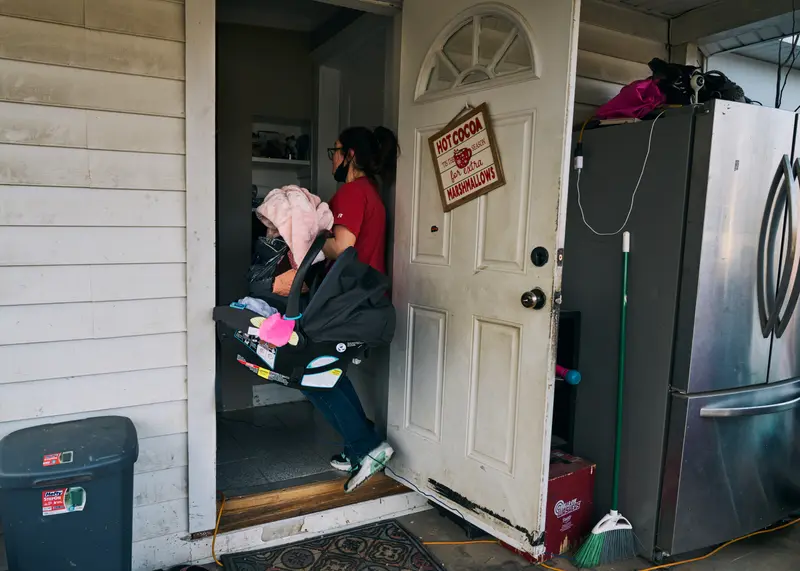
After four days, Hollis had to leave Elayna in the hospital and go home. There was no availability in charity housing for parents of NICU babies, and she needed to take care of Zooey.
Then, three days later, sheriff’s deputies showed up at Hollis’ door and took her to jail.
Though the child welfare case had been closed, now prosecutors were charging her with a felony over the same allegation that she left Zooey unattended in a car. She faced eight to 30 years in prison. She paid $6,000 in bail, erasing the savings she and her husband had hoped to use for parental leave. A judge’s order prohibited her from having any contact with Zooey, so her husband took over child care. With nowhere to go, Hollis spent the night in her car outside the hospital, going inside for Elayna’s feedings.



As Elayna’s lungs developed, her breathing improved. Every time Hollis managed to hold her daughter to her skin, her heart practically burst. She marveled at the fight inside such a small being and scribbled notes in a NICU progress book.
But her unrelenting challenges kept pulling her away. She and her husband quickly maxed out their $400 credit card limit on new legal fees and were down to a few dollars to pay for gas. Hollis knew she needed to get back to work.
Three weeks after Elayna’s birth, she returned to her job as an insulator apprentice and a punishing new routine: waking up at 4 a.m. to drive to the construction site an hour away, where she worked a 10-hour day for $16 an hour. Some evenings she went to school for her apprenticeship. Other nights she led an online Alcoholics Anonymous meeting to bolster her application for a peer recovery specialist certificate. She had finally been approved for housing near the hospital. Every chance she could, she ended the day with Elayna, but often she just had to catch up on sleep.
Then she got a call from the Department of Children’s Services. They were opening a new case because THC had been detected in Elayna’s umbilical cord. Hollis believed it was due to delta-8, a synthetic THC legal in Tennessee that doctors recommend avoiding during pregnancy. Hollis said she took it after the stress of her first hospitalization to help her sleep; she considered it less dangerous than the heavy antidepressant drugs her doctors had prescribed. Grimm wrote a letter to the department in her defense; he saw THC as a minor issue and emphasized her consistent negative tests for deadly drugs.
Sometimes, Hollis felt gripped with anger over her situation. The way she saw it, the same system that had forced her to risk her life offered little support to help her family stabilize in the aftermath. She wasn’t sure where to direct the blame, letting it spill out on her husband, other relatives and sometimes Grimm. She resented that she hadn’t understood enough about the law early enough to make a different decision. If she had been able to get an abortion, she thought, “my life could be so different right now.”

She heard that lawmakers were considering a change to the abortion law, to make it clear it was not a crime for doctors to provide abortion care in order to prevent life-threatening emergencies. “I’m so glad I have my baby,” she wished she could tell them. “But this was a risk I didn’t have any choice in taking.” She knew others wouldn’t be as lucky. On Tuesday, the state legislature is scheduled to consider bills aimed at creating clear medical exceptions. Tennessee Right to Life has strongly opposed it.
Elayna grew bigger and passed new milestones: Doctors found no bleeding in her brain. She began to breathe on her own and take in small amounts of milk. She was moved to a private room, where Hollis could sleep on a cot.
One night in early February, Hollis kissed Elayna, stretched out on the cot and tried to sleep amid the beeping, whirring and cries of babies in other rooms. Her mind was filled with worries about what life would look like once they left the safety net of the hospital, with its around-the-clock care and endless supply of formula and miniature diapers. She worried about managing it all, and about what could happen if she made another small mistake. She couldn’t bear losing either of her daughters and hadn’t even had a moment to process the loss of her uterus.
She drifted off and slept as the nurse fed the baby at midnight. Her iPhone alarm barely roused her at 3:30 a.m., time to get up for work.
On Feb. 23, the hospital told Hollis she could take her daughter home.
Elayna weighed four pounds and 12 ounces, still the size of one of Zooey’s dolls. Nurses removed all the wires attached to her and tested her to make sure she could keep her head up in her car seat. A nurse handed Hollis a stack of papers that contained instructions on feeding and bathing a premature baby and appointments for eye doctors, heart and liver specialists and neurological providers.
Hollis gently placed Elayna in her car seat and buckled her in. She tried to focus on today. It was Zooey’s first birthday, and the court had allowed them to live together again. Her husband was bringing home a cake and Hollis was desperate to have a moment to celebrate with her family. That night, relatives stopped by to greet the baby.


But about a week later, Elayna began showing signs of respiratory distress. One night, she suddenly stopped breathing. Hollis performed CPR until police officers arrived and saved Elayna’s life.
Two ambulance rides later, Elayna was airlifted to Vanderbilt. Over the following days, doctors found she had rhinovirus and outfitted her with a breathing machine. They told Hollis it was possible Elayna could have a bacterial infection, such as meningitis, in the fluid around her brain. To find out, they would need to do a spinal tap, but they worried it would destabilize her further. As Elayna’s condition worsened, Hollis wasn’t able to hold her because it might deplete her energy.
Hollis stayed as long as she could, but too much was waiting for her back home and she hated seeing her baby suffering. She whispered a quiet blessing and left Elayna in the pediatric intensive care unit, cocooned under the glow of a warming lamp.




Mariam Elba contributed research.
Photo editing by Andrea Wise.


















