By the time Cheryl Cosey learned she had COVID-19, she had gone three days without dialysis — a day and a half more than she usually waited between appointments. She worried how much longer she could wait before going without her life-saving treatments would kill her.
The 58-year-old Cosey was a dialysis technician for years before she herself was diagnosed with end-stage renal disease. After that, she usually took a medical transport van to a dialysis facility three days a week. There, she sat with other patients for hours in the same kind of cushioned chairs where she’d prepped her own patients, connected to machines that drew out their blood, filtered it for toxins, then pumped it back into their fatigued bodies.
Her COVID-19 diagnosis in the pandemic’s first weeks, after she’d been turned away from a dialysis facility because of a fever, meant Cosey was battling two potentially fatal diseases. But even she didn’t know how dangerous the novel coronavirus was to her weakened immune system.
Had she realized the risks, she would have had her daughter Shardae Lovelady move in. Just the two of them in Cosey’s red brick home on Chicago’s West Side, looking out at the world through the sliding glass door in the living room, leaving only for her dialysis.

After Cosey’s positive test in April 2020, Lovelady had to take her mother to a facility that treated patients with suspected or confirmed COVID-19. The facility fit her in for one of its last appointments the next day.
At that point, Cosey had gone more than four days without dialysis.
Four hours later, after Cosey completed her treatment, Lovelady returned to the nearly deserted building to bring her mother home, the sun having long disappeared from the sky. Cosey, dressed in a sweater and a green spring jacket, was disoriented, her breathing sporadic.
Alone with her mother on the sidewalk, Lovelady ran inside to ask workers for help getting Cosey out of her wheelchair and into her car.
“They offered no assistance,” Lovelady said. “They treated her as though she was an infection.”
(A spokesperson for the facility said employees aren’t allowed to help patients once they leave, for safety reasons.)
As Lovelady waited for paramedics to arrive, she grabbed a blanket from her car to wrap around her mother.
“My mother has COVID. I know she has COVID, but I didn’t care,” Lovelady said. “I hugged her and just held on until the ambulance came.”
Then she followed the flashing lights to the hospital.
In the three decades before the pandemic, the number of Americans with end-stage renal disease had more than quadrupled, from about 180,000 in 1990 to about 810,000 in 2019, according to the United States Renal Data System, a national data registry. About 70% of these patients relied on dialysis in 2019; the other 30% received kidney transplants.
The Midwest stood out as the region with the highest rate of patients with the disease, and Illinois had the nation’s third highest prevalence after Washington, D.C., and South Dakota, according to the Centers for Disease Control and Prevention.
A rare bright spot was the downturn in the death rate. Although diagnoses have been going up, death rates for patients who are on dialysis have declined since the early 2000s.
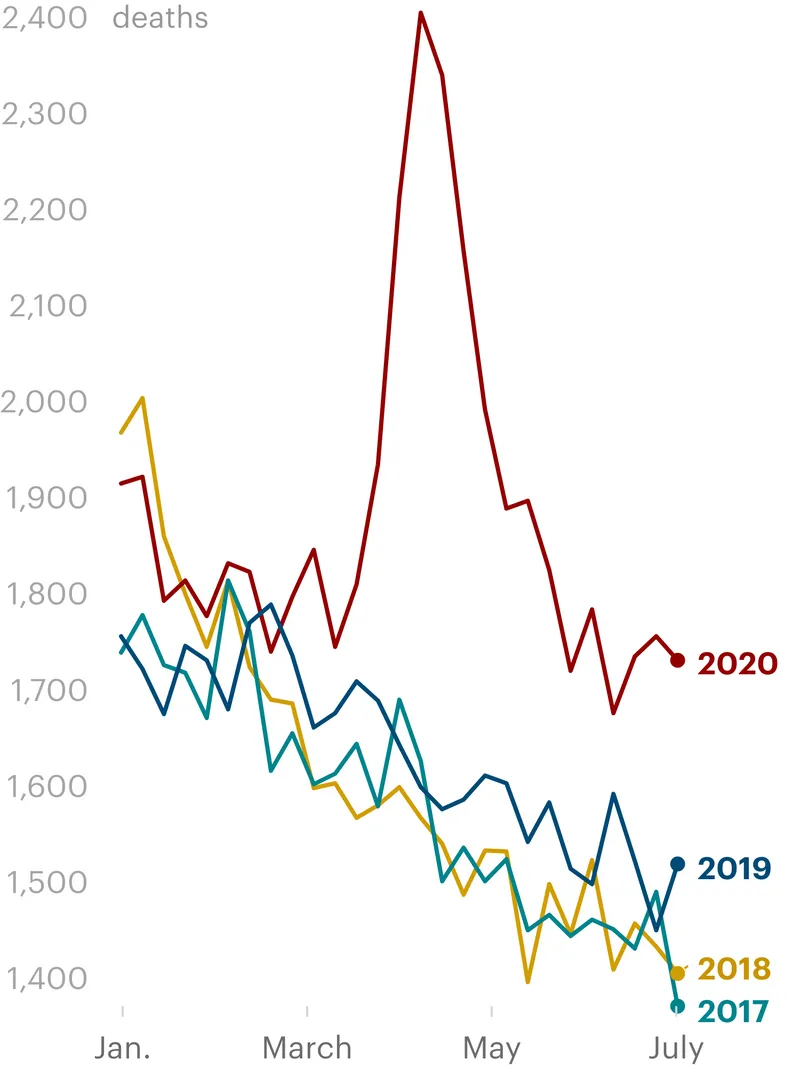
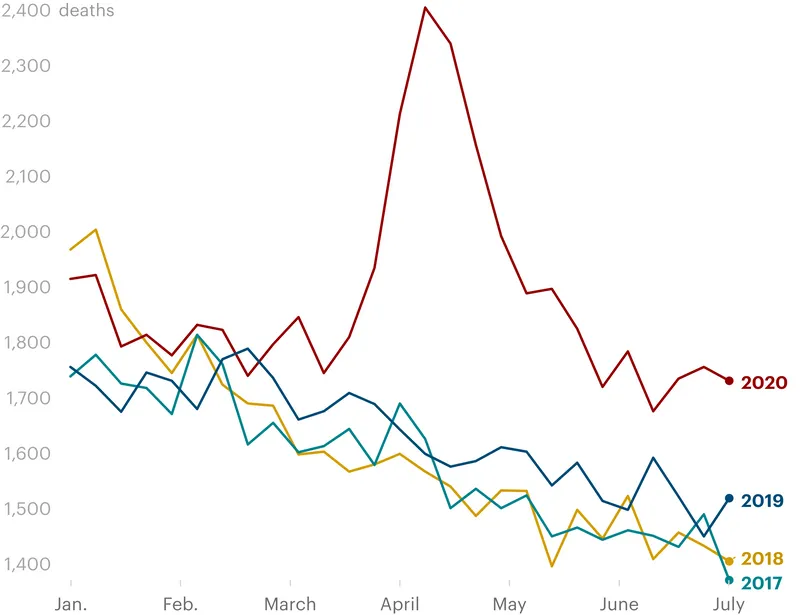
Then COVID-19 struck. Nearly 18,000 more dialysis patients died in 2020 than would have been expected based on previous years. That staggering toll represents an increase of nearly 20% from 2019, when more than 96,000 patients on dialysis died, according to federal data released this month.
The loss led to an unprecedented outcome: The nation’s dialysis population shrank, the first decline since the U.S. began keeping detailed numbers nearly a half century ago.
They were COVID-19’s perfect victims.
“It can’t help but feel like a massive failure when we have such a catastrophic loss of patients,” said Dr. Michael Heung, a clinical professor of nephrology at the University of Michigan. “It speaks to just how bad this pandemic has been and how bad this disease is.”
Before most patients reach advanced kidney failure, they are diagnosed with diabetes, hypertension or a host of other underlying conditions. Their immune systems are severely compromised, meaning they are essentially powerless to survive the most dangerous infections.
Many are old and poor. They also are disproportionately Black, as was Cosey. A 2017 study called end-stage renal disease “one of the starkest examples of racial/ethnic disparities in health.” Those inequities carried through to the pandemic. Dialysis patients who were Black or Latino, according to federal data, suffered higher rates of COVID-19 by every metric: infection, hospitalization, death.
Their deaths went largely unnoticed.
To get their treatments, the majority of dialysis patients in the U.S. must leave the relative safety of their homes and travel to a facility, often with strangers on public or medical transportation. Once at the dialysis center, they typically gather together in a large room for three to four hours.
The fear of contracting the virus was enough to keep many from venturing out for medical care, including those already on dialysis and those set to get the treatment for the first time. Exactly how long patients can go without dialysis depends on a number of factors, but doctors generally begin to worry if they miss two of their thrice-weekly sessions.
Dr. Kirsten Johansen, director of the United States Renal Data System, said the rates of people starting dialysis had been relatively stable until the pandemic. “Then the floor fell out,” she said in an interview.
COVID-19’s collateral damage played out in other ways as well. It meant that people delayed going to the hospital for everything from heart disease to cancer. For dialysis patients, whose life expectancy in some cases is three decades shorter than the general population, the results were calamitous. Hospitalizations of dialysis patients for reasons unrelated to COVID-19 dropped 33% between late March and April of 2020, federal data shows.
Dr. Delphine Tuot, a nephrologist and associate professor at University of California San Francisco and Zuckerberg San Francisco General Hospital and Trauma Center who focuses on vulnerable populations, found herself pleading with some of her patients to come in for their regular dialysis appointments.
One of them was a 60-year-old man whose shortness of breath landed him in the hospital in February. Doctors scheduled dialysis three times a week, and though he was initially resistant, Tuot said, he came around once he realized he would die without it.
Still, he missed appointments. When Tuot followed up, he told her he was afraid to leave the house because he was caring for his wife who had cancer, and he didn’t want to contract COVID and bring it home to her. Soon a cycle began. He skipped treatments, fluid built up in his body and an ambulance rushed him to the hospital because he couldn’t breathe. He got dialysis, was sent home and got back on track.
When cases surged and the delta variant took hold this summer, the cycle restarted — until he skipped dialysis for three weeks in a row, so long that his heart couldn’t recover, according to Tuot. He died last month.
Despite early efforts to mask and isolate patients at dialysis facilities, one study found the rate of COVID-19 hospitalizations of dialysis patients from March to April 2020 was 40 times higher than the general population.
Even with skyrocketing hospitalizations, it took three months after vaccines were approved before federal officials provided vaccinations to dialysis clinics, despite advocacy groups urging that this high-risk population be prioritized.
Although dialysis centers were swift to implement safety protocols in the pandemic’s early days, some facilities didn’t follow their own infection control policies, including washing hands properly, keeping workers home when sick or disinfecting equipment, federal inspection records show.
And home dialysis, which has been shown to be safer for patients during the pandemic, is out of reach for many, especially Black and Latino patients. Nephrologists had pushed for greater access to home dialysis before the pandemic; that need is more apparent now than ever, Tuot said.
“The fact that individuals had to go to a center with other individuals who are equally immunocompromised and had to get to that center, whether that was by public transportation or by van transportation, it’s clearly additional risks,” Tuot said. “Bottom line, they are very vulnerable. They’re very sick.”
The ambulance took Cosey to Chicago’s Rush University Medical Center. Lovelady filled in the staff on her mother’s medical history of end-stage renal disease, high blood pressure and asthma. The next day, Cosey called her daughter from her hospital bed. Lovelady noticed marked improvement from the night before.
“She sounded like herself,” Lovelady said. “We joked around a little bit. I asked her what kind of medicine she was on. She said they started her on dialysis.”
One by one, Lovelady added her sister, cousin and brother to the call. They told Cosey she had scared them, but now that she was doing better, they teased that they needed her to come home to bake her famous cheesecake. Her grandchildren hadn’t stopped asking about her either. They missed movie nights at Cosey’s house, when she made them popcorn and covered the floor with blankets.
Cosey’s boisterous laugh reassured them.
When Lovelady sensed her mother tiring, she told her she’d call her back the next day.
“Go ahead and get some rest,” she said.
Dialysis Patient Deaths Spiked in Early 2020
While the arrival of the pandemic rocked the health care system as a whole, the effect on dialysis facilities has received little attention.
The Centers for Medicare & Medicaid Services typically monitor the facilities through routine inspections and surprise visits to investigate specific complaints. But federal officials are two years overdue on more than 5,000 inspections at dialysis facilities across the country, Medicare data shows, and three years behind on more than 3,000 of them. Since the start of 2020, the number of inspections to dialysis facilities by government officials fell by more than 30% from the previous two years, ProPublica found. Complaints made up a larger portion of investigations. In 2019, 35% of total visits were in response to complaints. Last year, it jumped to 51%.
A spokesperson for the Centers for Medicare & Medicaid Services said in a statement that the pandemic forced the agency to temporarily suspend or delay inspections for non-urgent complaints and routine inspections to focus on infection control and critical concerns that placed patients in immediate jeopardy. The agency is working with states, which act on behalf of federal officials, to address the resulting backlog, the spokesperson said, but “nearly all state agencies report insufficient resources to complete the required, ongoing federal workload.”
The spokesperson said “the COVID-19 pandemic has presented a unique challenge unlike any other in history and has impacted our routine oversight work,” adding that “complaint investigations remain our first priority to ensure we address the immediate needs of patients receiving care in dialysis facilities.”
Insufficient funding has compounded those challenges. The budget for inspections has “been flatlined” since fiscal year 2015, while the number of dialysis facilities has increased by 21% to nearly 8,000 today, according to the agency. After several years of requesting more money, the centers were approved to receive an increase for fiscal year 2022.
When investigators did inspect dialysis facilities, they found some violations specific to COVID-19 and others that involved general safety lapses, according to federal records from March 2020 to July 2021.
A dialysis patient who started treatment just before the pandemic died after a nurse at a Kentucky facility failed to properly dilute an antibiotic, according to inspection reports. Minutes after the medicine began dripping through an IV, the patient said: “My body is on fire! It’s going through my whole body,” records show.
At a New York facility, another patient died after losing more than 1 1/2 pints of blood when their catheter became disconnected, according to federal records. That same facility underreported its number of deaths in the first 11 months of the pandemic by 16 people.
Federal officials issued their most serious citation to an Indiana facility for refusing to provide dialysis to a patient suspected of having COVID-19. The patient’s previous dialysis had also been cut short because their assisted living facility did not provide them transportation after 9:15 p.m. So they did not receive a complete treatment.
An estimated 5% to 10% of end-stage renal patients live in congregate settings, such as nursing homes or assisted living facilities. The same factors that led to nursing home populations being decimated — age, health, difficulty isolating — applied to those dialysis patients. In the first months of the pandemic, they contracted the virus at a rate more than 17 times higher than those who lived independently, according to one study.
Workers at those facilities weren’t immune either. Oluwayemisi Ogunnubi, 59, worked as a nurse administering dialysis to patients inside a nursing home on Chicago’s South Side. A Nigerian immigrant, she had sent money home to pay for her children’s schooling until she was able to bring them to the U.S. Her smile and supportive nature made her popular among her coworkers, according to an official at Concerto Renal Services, the dialysis company where she worked.
On April 21, 2020, Ogunnubi’s body began to ache, and she was sent home early from work. She was later taken to a hospital, where she tested positive for COVID-19. She died three days later, federal and county records show.
Occupational Safety and Health Administration officials cited Concerto, and levied a penalty of $12,145. The company provided employees who performed dialysis on patients with N95 respirators, but investigators found that Concerto’s written procedures weren’t complete and that the company had failed to provide medical evaluations that ensured employees knew how to use the respirators.
Two other Concerto employees, including one who fell ill the same day as Ogunnubi, contracted COVID-19 at the time but survived. Within two weeks of Ogunnubi’s death, 10 residents at the nursing home died of complications related to COVID-19, according to Cook County Medical Examiner records. Half had kidney failure.
Kyle Stone, Concerto’s executive vice president and general counsel, said the first and only COVID-related death of an employee shook the company. Stone said Concerto “made a difficult choice” to use respirator masks without providing medical evaluations to employees, but it “was clearly the correct choice under the circumstances.”
If Concerto had been required to fulfill every aspect of OSHA requirements for a written policy that early in the pandemic, he said, the company would not have been able to provide the respirator masks, “almost certainly resulting in greater risk of harm and death.”
OSHA’s failure to “see and appreciate” the trying circumstances at the time, Stone said, was “baffling and disappointing.” Concerto eventually settled with OSHA, which downgraded the violation and reduced the penalty to $9,000.
“We are quite proud of our work in 2020 during the eye of the COVID storm,” Stone said.
As devastating as the pandemic has been, many experts say it could have been worse. Dr. Alan Kliger, a clinical professor of medicine at Yale School of Medicine, co-chaired the American Society of Nephrology COVID-19 Response Team that held weekly calls with chief medical officers from 30 or so dialysis companies, including the largest two, DaVita and Fresenius. The facilities, Kliger said, implemented universal masking and patient screenings before the CDC recommended them. They also treated COVID-19 patients in separate shifts or at specifically designated isolation clinics.
“There’s been a tremendous amount of collaboration and sharing of information and uptake of best practices in this group of competitive companies,” Kliger said. “They really rallied together to protect patients.”
Epidemiologist Eric Weinhandl said that there’s another battle on the horizon with the omicron variant spreading rapidly, which he finds especially worrisome given how federal officials failed by not distributing vaccines to dialysis facilities in December 2020.
“It’s heartbreaking because you look at this, and much like nursing home residents, these patients are completely vulnerable. But they still have to go to a dialysis facility three times a week,” Weinhandl said. “Why wouldn’t you prioritize this population?”
The CDC said in a statement that “demand exceeded supply” when vaccines were first authorized and “as supply increased and states adopted CDC’s recommendations, older adults and those with underlying health conditions began being prioritized.”
It wasn’t until March 25 that the Biden administration announced it was partnering with dialysis facilities to send vaccines to patients at the centers.
Now, Weinhandl wonders if dialysis patients will be a priority if the federal government approves a second round of boosters for high-risk patients.
“Is there a plan? Because I think that there should be,” he said. “I think this is getting pretty predictable. Every time COVID surges, you see the dialysis population’s excess mortality surge with it.”
Sometimes the frailty of dialysis patients is no match for COVID-19’s brutality.
Oscar and Donna Perez were the kind of siblings who loved each other without judgment or condition. After Oscar began dialysis in 2018, Donna picked him up from his appointments three nights a week. She cut his toenails when his feet were too swollen for him to reach and massaged them when the pain woke him up at night.
He was her son’s godfather, her best friend who shared his love of music with her — especially the 1960s R&B singer Billy Stewart — and annoyed her in the way only brothers can, swatting her feet off chairs just as she got comfortable and pestering her with questions when she was deep into Instagram.

But Oscar Perez was sick. In addition to his failing kidneys, the 38-year-old Latino father struggled with hypertension, diabetes and congestive heart failure. In early January, doctors performed coronary bypass surgery. He was not yet eligible for the vaccine, but the hospital tested him for COVID-19 when he was admitted. He was negative.
He went home on Jan. 18, the same day as the wake for his uncle, who, his family said, died after he missed too many dialysis appointments. But the next day, Oscar collapsed at home, confused and mumbling in pain, with signs that the coronavirus was flourishing in his lungs. He was rushed back to the hospital. A doctor called to tell Donna Perez that her brother had tested positive and needed to be intubated.
On Jan. 31, doctors called Donna again and told her that her brother’s condition was declining fast. She picked up her parents, another brother and his girlfriend, and headed to the hospital to visit Oscar from outside the glass door of his room. They told doctors to try to resuscitate him if his heart stopped.
That night, after they returned home, Donna Perez’s phone rang one more time. Oscar’s doctor said he probably wasn’t going to make it through the night. This time, they could visit him in his hospital room in PPE.
Seeing her brother up close, swollen and helpless, she leaned in, hugged him, and said, “I can tell you’re tired. You can go.” Donna promised to take care of his daughter.
Her family pushed back and said she had to tell him to be strong.
Donna told them they needed to let Oscar go. He died a few hours later.
“This disaster is one that befalls dialysis patients, with diabetes especially, regularly,” Dr. David Goldfarb, clinical director of the nephrology division at NYU Langone Health in New York City, who reviewed Oscar Perez’s medical records for ProPublica.
“Of course, it’s possible to do better,” he continued. “Given his age, it’s really tragic.”
The advent of technology to filter a patient’s blood revolutionized kidney care in the 1950s, and people lined up to get access to the limited number of machines. In 1960, one hospital created its own admissions panel, later nicknamed the “God committee,” to review cases to decide who would receive the groundbreaking treatment.
Twelve years later, Congress approved legislation that created the Medicare End Stage Renal Disease program, which guaranteed coverage of medical care, including dialysis and kidney transplants. It remains the only disease-specific Medicare entitlement program, credited by some as possibly saving more lives than any other federal government program. Generally, Medicare only covers those over age 65 and the disabled, but this program is available to people of all ages with end-stage renal disease.
Total Medicare-related spending in 2019 on end-stage renal disease patients topped $50 billion. Even with that budget, the agency hasn’t been able to fix persistent health disparities. That year, Black patients were more than four times more likely than their white counterparts to have the disease.
Black patients also progressed from chronic kidney disease to end-stage renal disease three times as often as white patients. Yet they are less likely to start off their dialysis treatments on a waiting list for a transplant — or eventually receive one from a living donor — than white patients.
In a statement, Medicare said it is working to address the disparities and said it is “committed to ensuring the health and safety” of all its dialysis patients.
Another area of concern is home dialysis, which research has shown is cheaper than in-center dialysis and offers similar or better survival rates, enhanced quality of life and greater flexibility. Barriers to home dialysis affect all patients, but the percentages of Black and Hispanic patients receiving home dialysis in 2019 were 10% and 11% respectively, compared with white and Asian patients at 17% each.
The push for closing that gap has gained traction, bolstered by federal data that found COVID-19 hospitalizations rates of patients who underwent home dialysis from late March to June 2020 were between one-quarter and one-third those of patients traveling to dialysis facilities.
“We do have to figure out a way to do better because we’re really, in essence, causing harm, when we’re not able to divert proper resources to patients who most require them,” said Dr. Kirk Campbell, a nephrology professor and vice chair of medicine for diversity, equity and inclusion at the Icahn School of Medicine at Mount Sinai in New York City.
Some patients don’t have the space to store the supplies needed for home dialysis. Others are overwhelmed by the prospect of having to keep the area around the catheter clean to prevent infection. But, Campbell said, that’s where patient education comes in. The most common type of home dialysis, called peritoneal dialysis, often is done at night while the patient is sleeping and does not involve blood flowing outside the body.
While home dialysis isn’t possible for all patients, some doctors are hesitant to recommend it at all, in part because the clinicians lack the training, experience or a certain comfort level with it. That’s especially true, Campbell said, for patients of color and those from disadvantaged backgrounds. There’s often an unconscious bias that those patients won’t be able to handle it, he said.
Campbell and others said it’s critical that clinicians receive additional training in home dialysis. He leads one of the few nephrology fellowship programs in the country where doctors can spend an extra year specializing in home dialysis. The results have been so promising, he said, that they hope to expand.
In July 2019, the Trump administration issued an executive order aimed at revamping kidney care in the United States through the Department of Health and Human Services’ Advancing American Kidney Health initiative. The goals of the initiative were lofty — some say unrealistic — and included having 80% of new end-stage renal disease patients in the U.S. receive in-home dialysis or transplants by 2025. In 1972, the year the Medicare program passed, 40% of patients were on home dialysis. Currently, about 13% of patients are receiving dialysis at home.
Starting January, the Centers for Medicare & Medicaid Services will offer facilities greater reimbursement for improving their home dialysis rates for low-income patients.
Some observers say the change doesn’t go far enough. In September, U.S. Rep. Bobby Rush, an Illinois Democrat, and Rep. Jason Smith, a Republican from Missouri, proposed legislation that would require Medicare to pay for workers to assist patients who need additional help with home dialysis. The measure, which was introduced without much fanfare, also calls for greater patient education around the treatment and a federal study analyzing racial disparities.
Hong Kong, where about three in four patients are on peritoneal dialysis, is a global leader in home treatment. Patients there receive peritoneal dialysis first unless there is a medical reason that would preclude it.
Dr. Isaac Teitelbaum, a nephrologist who has been the medical director of the home dialysis unit at the University of Colorado School of Medicine since 1986, said expanded training for clinicians and incentives for patients, including a reduced co-pay or a tax credit, could encourage more patients to dialyze at home.
“You don’t live just so you can do dialysis. You do dialysis so that you can enjoy life,” he said. “You do dialysis so that you can watch your children and grandchildren grow up and so that you can participate in family events and go on vacations.”
Cheryl Cosey was not offered home dialysis, her family said. Shardae Lovelady said it might have made all the difference for her mother.
Cosey’s health deteriorated quickly after the call from her hospital bed. Doctors transferred Cosey to the intensive care unit, put her on a ventilator and gave her medication to push the oxygen from her lungs into her bloodstream, according to hospital records.
The family braced themselves. Lovelady drove to Minnesota to pick up her sister. She gathered everyone for a big dinner the way her mother used to do.
Lovelady and her sister stayed up late talking, finally dozing off when the house quieted.
When the phone rang at three in the morning, Lovelady recognized the hospital’s 312 area code.
Everything she had done to prepare for that moment suddenly vanished, and she allowed herself to hope.
The call was short. She never even flipped on the bedroom light. She turned to her sister, who was asleep next to her, and nudged her awake.
“Mama gone.”